The Ulnar Nerve grows within the axilla from the medial cord of brachial plexus (C8 and Tl). The ventral ramus of C7 contributes to the ulnar nerve. The C7 fibers in the ulnar nerve supply flexor carpi ulnaris.
Course of Ulnar Nerve
Axilla
The nerve lies medial to 3rd part of axillary artery (between axillary artery and vein).
It runs distally along the medial side of the brachial artery as much as the midarm (level of insertion of coracobrachialis) and goes into the armas part of primary neurovascular package. To go into the posterior compartment of the arm, it penetrates the medial intermuscular septum and runs downwards to the opposite side of the medial epicondyle of humerus. On the opposite side of the medial epicondyle, it is sticked in a canal or groove where it can be quickly palpated. The transformation of the groove into a tunnel takes place, which is called cubital tunnel by a fibrous band extending between medial epicondyle and olecranon process. In the flooring of the tunnel, the ulnar nerve crosses the ulnar collateral ligament.
The ulnar nerve does not offer any branch in the axilla and in the arm near ulna bone.
Forearm
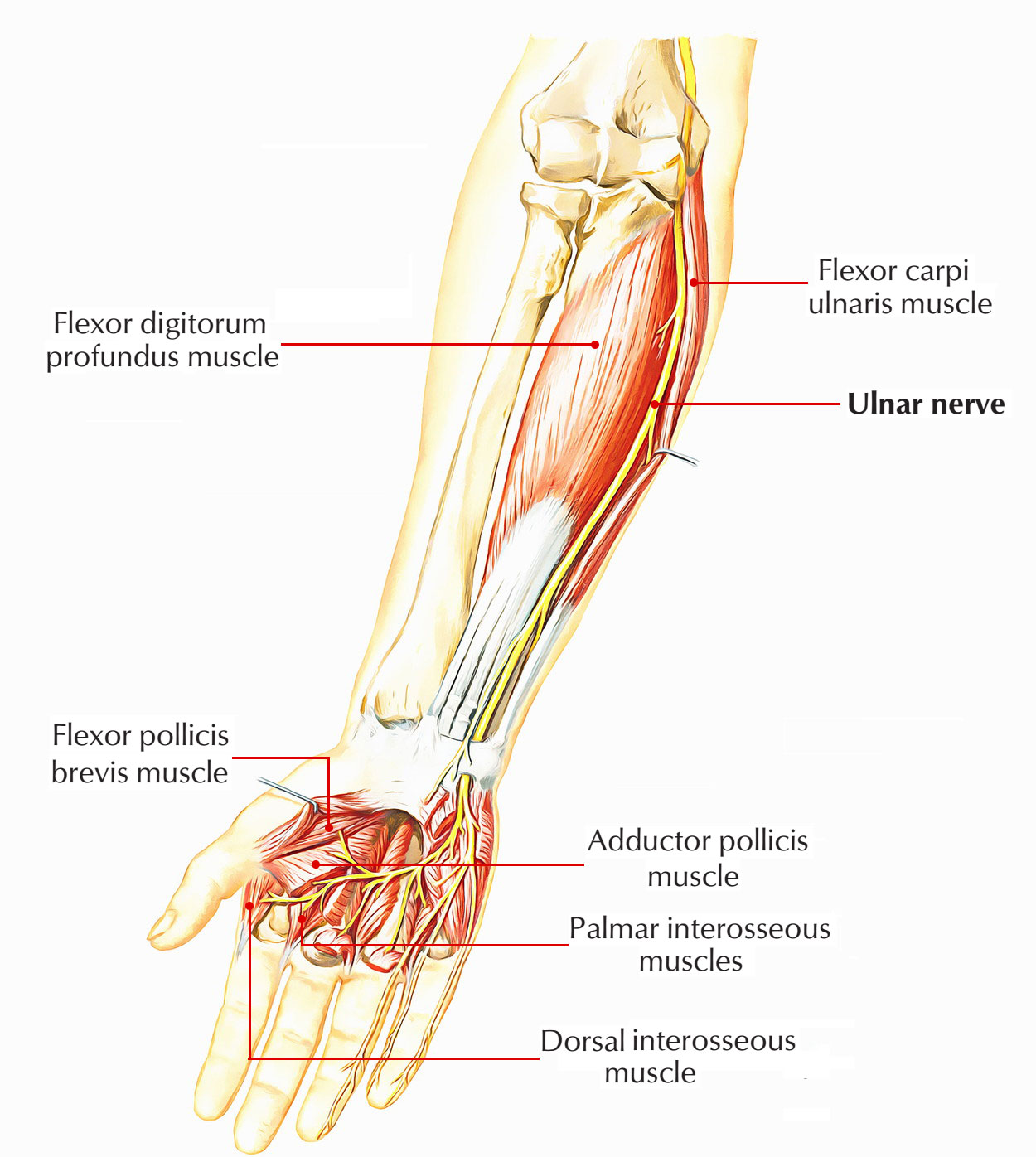
The nerve goes into the forearm by passing between the 2 heads of flexor carpi ulnaris. In the upper third of forearm, it runs practically vertically downwards under flexor carpi ulnaris. In the lower two-third of the forearm, it ends up being superficial and lies lateral to the flexor carpi ulnaris. In this part of its course the ulnar nerve and artery come down together, artery being on the lateral side of the nerve.
In the forearm, it produces the following branches:
- In the proximal forearm, it supplies muscular branches to flexor carpi ulnaris, and medial half of flexor digitorum profundus.
- In the mid-forearm, it produces palmar cutaneous branch, which goes into the palm superficial to the flexor retinaculum to supply sensory innervation to the skin over the hypothenar eminence.
- In the distal forearm, about 5 cm proximal to the wrist, it produces dorsal cutaneous branch which offers sensory innervation to the skin over the medial 3rd of the dorsum of the hand and medial 1.5 finger.
Ulnar Nerve
Palm
The ulnar nerve goes into the palm by passing superficial to the flexor retinaculum lying simply lateral to the pisiform. Here the ulnar nerve is covered by a fascial band (volar carpal ligament).The space under this fascial band is described ulnar tunnel Simply distal to pisiform, the ulnar nerve divides into its terminal superficial and deep branches. The superficial terminal branch supplies palmaris brevis offers sensory innervation to the skin on the palmar surface of medial 1.5 fingers.
The deep terminal branch goes into Guyon’s canal(Piso hamate tunnel) under cover of Piso hamate ligament and turns laterally within concavity of deep palmar arterial arch and ends within substance of adductor pollicis which it supplies. The deep branch of ulnar nerve is simply motor and supplies all the intrinsic muscles of the hand other than the muscles of thenar eminence and very first 2 lumbricals.
The ulnar nerve behind medial epicondyle of humerus is described as ‘funny bone‘ due to the fact that when the medial part of the elbow strikes a tough surface, tingling feelings happen along the ulnar side of the forearm and hand.
The ulnar nerve is frequently described as ‘nerve of fine movements‘/’artist’s nerve‘ due to the fact that it innervates the majority of the intrinsic muscles of the hand that are associated with the great elaborate hand movements as needed by the artists while playing musical instruments.
Clinical Significance
Injuries of the Ulnar Nerve
The ulnar nerve is frequently hurt at 2 sites: (a) at elbow and (b) at wrist.
Injury of the ulnar nerve at elbow: The injury of ulnar nerve at elbow might happen due to:
- Fracture, dislocation of the medial epicondyle.
- Thickening of the fibrous roof of the cubital tunnel (cubital tunnel syndrome).
- Compression between the 2 heads of flexor carpi ulnaris (FCU) muscle.
- Valgus defect of elbow (tardy or late ulnar nerve palsy).
Particular clinical functions in such cases will be as follows:
- Atrophy and flattening of hypothenar eminence.
- Claw-hand defect (primary engriffe) impacting ring and little fingers. The very first phalanges of these fingers are extended and middle and distal phalanges are bent. It is not a real claw hand.
- Loss of abduction and adduction of fingers.
- Flattening of hypothenar eminence and depression of interosseous areas on dorsum of hand due to atrophy of interosseous muscles, respectively.
- Loss of adduction of thumb.
- Loss of sensation over the palmar and dorsal surfaces of the medial 3rd of the hand and medial 11/ 2 fingers.
- Foment’s indication is positive.
Injury of the ulnar nerve at wrist: The ulnar nerve at wrist is hurt due to
- Superficial position of ulnar nerve at this site makes it susceptible to cuts and injuries.
- Compression in the Guyon’s canal/Piso hamate tunnel.
Particular clinical functions in such cases will be as follows:
- Claw-hand defect impacting ring and little fingers (ulnar claw hand) however it is more noticeable (ulnar paradox) due to the fact that the FDP is not disabled; for that reason there is a significant flexion of DIP joints.
- Atrophy and flattening of hypothenar eminence.
- Loss of abduction and adduction of fingers.
- Foment’s indication is positive.

 (46 votes, average: 4.63 out of 5)
(46 votes, average: 4.63 out of 5)