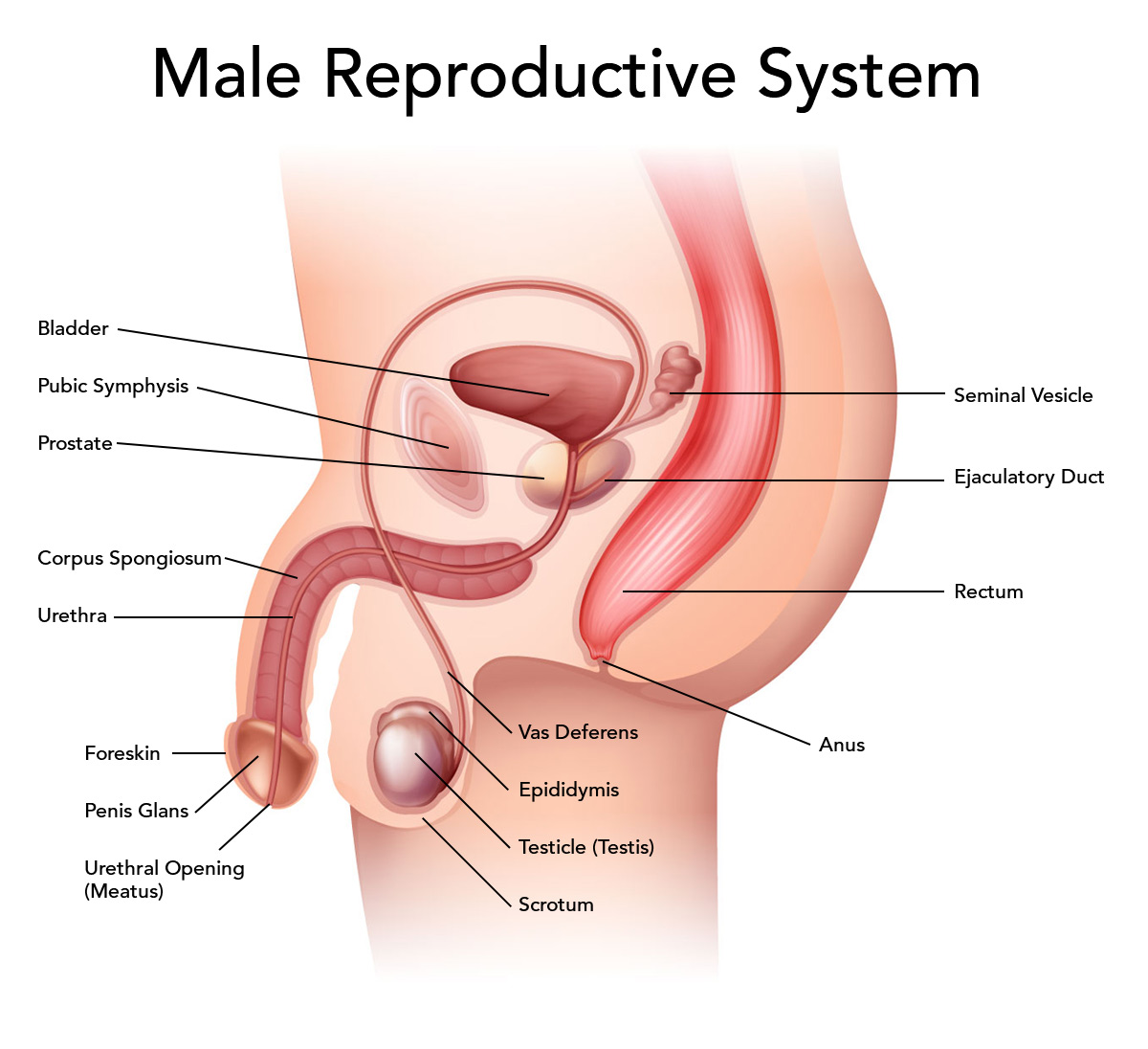
The primary functions of the male reproductive system are the production of male sex hormones, the formation of sperm, and the placement of sperm in the female reproductive tract, where one sperm can unite with a female sex cell. The organs of the male reproductive system include (1) paired testes, which produce sperm and male sex hormones; (2) accessory ducts that store and transport sperm; (3) accessory glands, whose secretions form part of the semen; and (4) external genitalia, including the scrotum and penis.
Male Reproductive System
Testes
The paired testes (tes ‘-tez, singular, testis) are the male gonads, or sex glands. Each testis is protected and
supported by a capsule of dense irregular connective tissue. Septa (partitions) of connective tissue radiate into the testis from its posterior surface, dividing the testis into internal subdivisions called lobules. Each lobule contains several highly coiled seminiferous (se-mi-nif’-er-us) tubules. Seminiferous tubules are lined with spermatogenic epithelium, which is formed of spermatogenic cells and supporting cells. Spermatogenic cells divide to produce sperm, while supporting cells support and nourish the spermatogenic cells and help regulate sperm formation. The cells that fill the spaces between the seminiferous tubules are known as interstitial (in-ter-stish’-al) cells, and they produce male sex hormones.
Spermatogenesis
Spermatogenesis (sper-mah-to-jen’-e-sis) is the process that produces sperm by the division of the spermatogenic cells in the spermatogenic epithelium. Spermatogenesis begins at puberty (pu’-ber-te), the age at which reproductive organs mature, and continues throughout the life of a male. Sexual maturity and sperm production are controlled by follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior lobe of the pituitary and by testosterone from interstitial cells of the testes. LH is often called interstitial cell-stimulating hormone (ICSH) in males.
The large, superficial cells near the basement membrane of a seminiferous tubule are known as spermatogonia (singular, spermatogonium). Each spermatogonium contains 46 chromosomes (23 pairs), the normal number of chromosomes for human body cells. Each spermatogonium divides by mitosis to produce two spermatogonia, referred to as type A and type B spermatogonia, each with 46 chromosomes. The type A spermatogonium remains next to the basement membrane of the tubule. It will serve as the “stem” spermatogonium and will divide repeatedly by mitosis. The type B spermatogonium that is pushed toward the lumen of the tubule undergoes changes to become a primary spermatocyte.
Primary spermatocytes divide by meiosis (mi-o’-sis), a special type of cell division. Meiosis requires two successive divisions and reduces the number of chromosomes in the daughter cells by one-half.
Each primary spermatocyte, containing 46 chromosomes, divides in meiosis I to form two secondary spermatocytes, each containing 23 chromosomes. Prior to meiosis I, the chromosomes replicate. Each replicated chromosome is composed of two chromatids joined together at a region called a centromere. During metaphase of meiosis I, the replicated chromosomes are arranged as homologous pairs. During cytokinesis, the members of each chromosome pair are separated into different daughter cells. Thus, each secondary spermatocyte contains 23 replicated chromosomes.
The genetic diversity of the sperm is created by the following two mechanisms. First, random alignment of the paired homologous chromosomes on the cellular equator occurs during meiosis I, so that the daughter cells contain different combinations of maternal and paternal chromosomes. Second, crossover, the exchange of some DNA between the paired homologous chromosomes, occurs during meiosis I, so that some chromosomes contain genes from both parents.
In meiosis II, the chromatids separate into different daughter cells so each secondary spermatocyte divides to form two spermatids, each containing 23 chromosomes. Each spermatid attaches to a supporting cell, gradually loses much of its cytoplasm, and develops a flagellum to form a sperm containing 23 chromosomes.
Note how cells in stages of spermatogenesis are arranged in sequence from superficial to deep, with sperm located in the lumen of the tubule. Once the sperm are completely formed, they are carried into the epididymis, where they are temporarily stored while they mature.
A mature sperm consists of a head, neck, and flagellum. The flattened head is composed of a compact nucleus containing 23 chromosomes. The anterior portion of the head is covered by a caplike structure, the acrosome. The acrosome contains enzymes that help the sperm penetrate a female sex cell. The neck connects the head to the flagellum. The flagellum has a middle piece, a principal piece, and an end piece. The middle piece contains mitochondria, where ATP is formed to power the movements of the flagellum, which enables movement.
Accessory Ducts
Sperm pass through a series of accessory ducts as they are carried from the testes to the external environment. These accessory ducts include the epididymis, vas deferens, ejaculatory duct, and urethra. These structures are collectively referred to as the male reproductive tract.
Epididymis
The seminiferous tubules of a testis lead to a number of small ducts that open into the epididymis. The epididymis (ep-i-did’-i-mis, plural, epididymides) appears as a comma-shaped organ that lies along the superior and posterior margins of a testis. Upon close examination, the epididymis is shown to be a long (6 m), tightly coiled, slender tube that is continuous with the vas deferens.
Sperm mature as they are slowly moved (10-14 days) through the epididymis by weak peristaltic contractions. The mature sperm are stored in the epididymis until they are ejaculated. The sperm stored for more than two months are destroyed and absorbed by the epididymis.
Vas Deferens
A vas deferens (vas def’-er-enz, plural, vasa deferentia) extends from the epididymis superiorly in the scrotum, passes through the inguinal canal, and enters the pelvic cavity. It runs along the lateral surface of the urinary bladder and merges with the duct from a seminal vesicle inferior to the urinary bladder. The duct formed by this merger is an ejaculatory duct. The vasa deferentia have rather thick, muscular walls that move the sperm by peristalsis.
Ejaculatory Duct
Each short ejaculatory duct is formed by the merger of a vas deferens and a duct from a seminal vesicle. The ejaculatory ducts enter the prostate gland and merge with the urethra within the prostate. During ejaculation, muscular contractions of the ejaculatory ducts mix seminal vesicle secretions with sperm and propel them into the urethra.
Urethra
The urethra is a thin-walled tube that extends from the urinary bladder through the penis to the external environment. The urethra serves a dual role in the male. It transports urine from the urinary bladder during micturition and it also carries semen, which includes sperm, during ejaculation. Control mechanisms prevent urine and semen passing at the same time.
Accessory Glands
Three different types of exocrine glands produce secretions involved in the reproductive process. These glands are the seminal vesicles, prostate gland, and bulbo-urethral glands.
Seminal Vesicles
The seminal vesicles are paired glands located on the posterior surface of the urinary bladder. The duct of each
seminal vesicle merges with the vas deferens on the same side to form an ejaculatory duct near the posterior surface on the prostate gland. The alkaline secretions of the seminal vesicles help to keep semen alkaline and contain fructose and prostaglandins. Secretions by the seminal vesicles compose about 60% of semen.
Prostate Gland
The prostate gland is a pear-shaped gland that encircles the urethra where it exits the urinary bladder. The ejaculatory ducts pass through the posterior portion of the prostate to join with the urethra within the prostate. Prostatic fluid is forced through 20 to 30 tiny ducts into the urethra during ejaculation. The secretion is an alkaline, milky fluid containing substances that activate the swimming movements of sperm. It forms about 30% of semen.
Bulbo-Urethral Glands
The bulbo-urethral (bul-bo-u-re’-thral) glands are two small, spherical glands that are located inferior to the prostate gland near the base of the penis. These glands secrete an alkaline, mucuslike fluid into the urethra in response to sexual stimulation. This secretion neutralizes the acidity of the urethra and lubricates the end of the penis in preparation for sexual intercourse.
Semen
The semen (se ‘-men) is the fluid passed from the urethra during ejaculation. It consists of the fluids secreted by the bulbo-urethral glands, seminal vesicles, and prostate gland along with sperm and fluid from the testes. The alkalinity (pH 7.5) of semen protects the sperm by neutralizing the acidity of the male’s urethra and the female’s vagina. Fructose from seminal vesicles provides the nutrient energy for sperm, and prostatic fluid activates their swimming movements. After semen is deposited in the vagina during sexual intercourse, prostaglandins in seminal vesicle secretions stimulate reverse peristalsis of the uterus and uterine tubes, which accelerates the movement of sperm through the female reproductive tract. The volume of semen in a single ejaculation may vary from 2 to 5 ml, with 50 to 150 million sperm per milliliter. Although only one sperm participates in fertilization, many sperm are necessary for fertilization to occur.
Male External Genitalia
Male external genitalia are the visible parts of the male reproductive system, including the scrotum and penis.
Scrotum
The scrotum (skro’-tum) is the external sac of skin and subcutaneous tissue that contains the testes. It hangs from the trunk midline posterior to the penis. A medial partition keeps each testis in a separate chamber within the scrotum. Testes develop within the pelvic cavity but descend into the scrotum through the inguinal canals near the end of the seventh month of fetal development. This migration occurs under the stimulation of testosterone. The descent of the testes into the scrotum keeps their temperature 2-3°F below average body temperature. This lower temperature is necessary for the production of viable sperm.
The subcutaneous tissue of the scrotum contains a layer of smooth muscle called the dartos. Its cells reflexively contract or relax to shorten or lengthen the scrotum in response to temperature changes. In addition, there are two thin, ribbon-like skeletal muscles, named cremaster, that are attached to the testes and respond similarly. Through the actions of these muscles, the testes are elevated closer to the body in cold temperatures and depressed in warm temperatures.
Penis
The penis is the male copulatory organ that deposits semen in the female vagina during sexual intercourse. It contains specialized erectile tissues that enable it to become enlarged and rigid during sexual excitement.
Three columns of erectile tissue compose the body of the penis. The corpora cavernosa are two columns located on the superior side of an erect penis. The single corpus spongiosum, through which the urethra extends, is located on the inferior side of an erect penis. The corpus spongiosum expands at the tip to form the glans penis, which contains numerous sensory receptors and the external urethral orifice. A loose sheath of skin, the prepuce, extends distally to cover the glans.
Summary of Functions of Male Reproductive Organs
| Organ | Function |
| Testis | Seminiferous tubules produce sperm and secrete inhibin; interstitial cells secrete testosterone |
| Epididymis | Site of sperm maturation and temporary storage; carries sperm to vas deferens |
| Vas deferens | Carries sperm to ejaculatory duct |
| Ejaculatory duct | Carries sperm and secretions from the seminal vesicle to the urethra |
| Urethra | Carries semen to the external environment |
| Bulbo-urethral gland | Secretes watery fluid that neutralizes acidity of the urethra and lubricates the glans penis |
| Seminal vesicle | Secretes alkaline fluid containing nutrients for sperm and prostaglandins for stimulating reverse peristalsis of the uterus and uterine tubes; helps keep semen slightly alkaline |
| Prostate gland | Secretes alkaline fluid that helps keep semen slightly alkaline and activates motility of sperm |
| Scrotum | Contains and protects testes; regulates temperature of testes |
| Penis | Inserted into vagina during sexual intercourse; deposits semen in vagina; contains sensory receptors associated with feelings of sexual pleasure |

 (54 votes, average: 4.63 out of 5)
(54 votes, average: 4.63 out of 5)