Synonyms: Ren: kidney (in Latin); Nephros: kidney (in Greek).
Kidneys are the two reddish-brown organs inside the abdomen, situated on the posterior abdominal wall, resembling beans.
The waste products of protein metabolism are removed by the kidneys and are therefore, these are known as the major excretory organs. Also, surplus of water and salts from the blood and are so necessary for preserving the electrolyte and water balance in the tissue fluids of the body, essential for survival.
Kidneys
Location
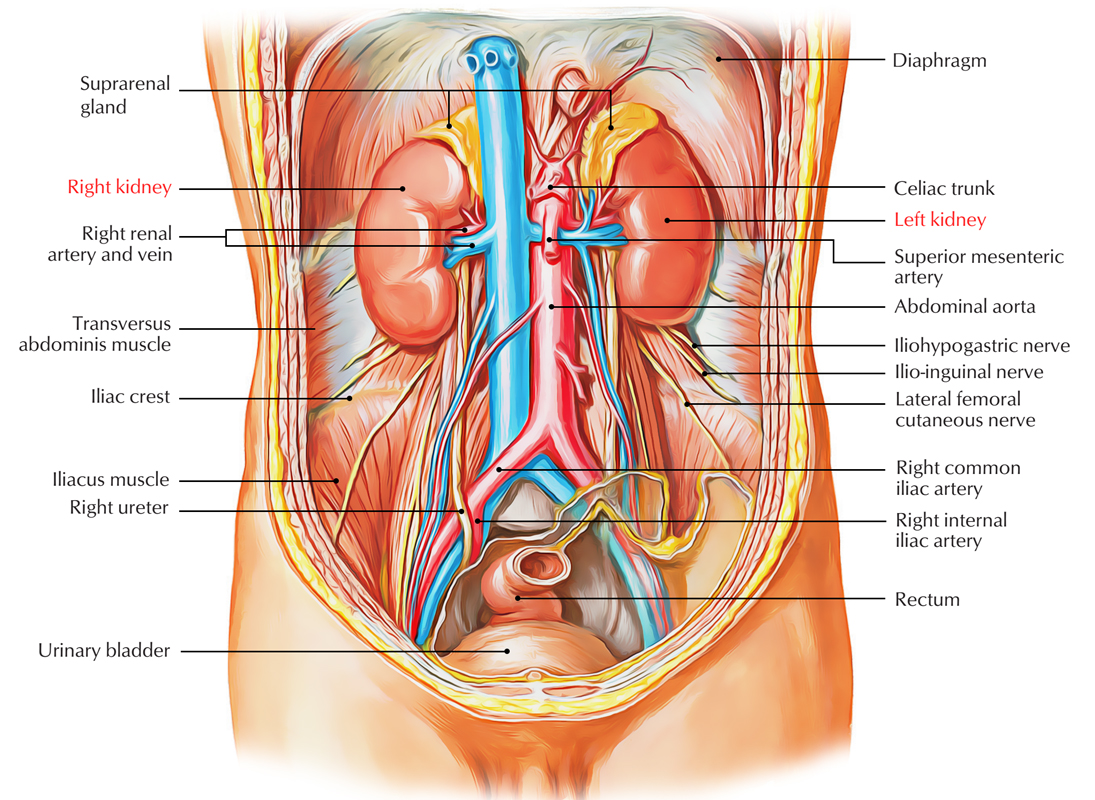
The kidneys be located on the posterior abdominal wall, 1 on every side of the vertebral column, behind the peritoneum, opposite 12th thoracic and upper 3 lumbar (T12 L3) vertebrae. They reside in epigastric, hypochondriac, lumbarand umbilical regions.
Kidneys: Location
- The right kidney is located at a somewhat lower level compared to the left 1 because of the presence of liver on the right side.
- The left kidney is little nearer to the median plane compared to the right.
- Their long axes are somewhat oblique (being pointed downward and laterally) so that their upper ends or Poles are nearer to every other than the lower Poles. The upper Poles are 2.5 cm far from the mid line, the hilum are 5 cm far from the mid line, and the lower Poles are 7.5 cm far from the mid line.
- Both kidneys move downward in vertical direction for 2.5 cm during respiration.
- Transpyloric plane goes through the upper part of the hilum of the right kidney and via the lower part of the hilum of the left kidney.
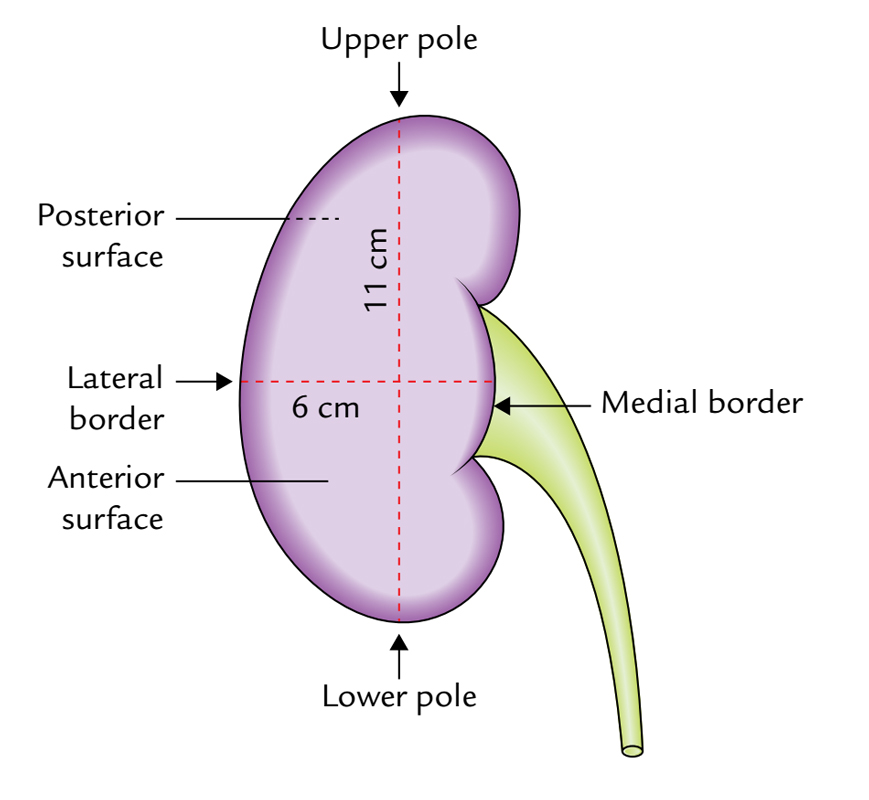
Shape and Measurements
Shape:
Legume shaped.
Measurements:
- Length: 11 cm. (left kidney is somewhat longer and narrower).
- Width: 6 cm.
- Thickness: (anteroposterior) 3 cm.
- Weight. 150 grams in men; 135 grams in females.
External Features
Kidneys: External Features
Every kidney presents the following external features:
- 2 Poles (superior and inferior).
- 2 surfaces (anterior and posterior).
- 2 edges (medial and lateral).
- A hilum.
Poles
- The superior (upper) post is thick and round and is located nearer to the median plane in relation to the inferior post. It’s related to the suprarenal gland.
- The inferior (lower) post is thin and pointed and is located 2.5 cm above the iliac crest.
Surfaces
- The anterior surface is convex and faces anterolaterally.
- The posterior surface is flat and faces posteromedially. Nonetheless, in practice it’s hard to comprehend anterior and posterior surfaces. This nevertheless is done easily by viewing the association of structures present at the hilum (vide infra).
Borders
- The medial border of every kidney is convex above and below near the Poles and concave in the middle. It slopes downward and laterally, and presents a vertical fissure in its middle part named hilum/hilus which has anterior and posterior lips.
- The lateral border of every kidney is convex.
Hilum
The medial border (central part) of the kidney presents a deep vertical slit named hilum. It conducts, from before backwards, these structures:
- Renal vein.
- Renal artery.
- Renal pelvis.
- Auxiliary branch of renal artery.
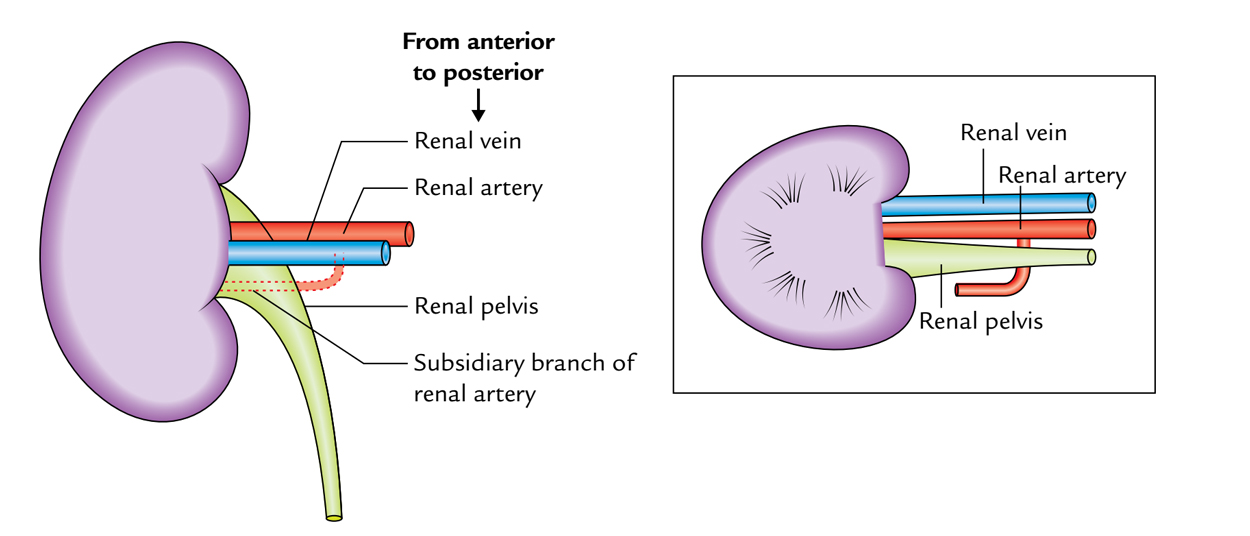
Kidneys: Hilum
Along with the above structures the hilum also conducts lymphatics and nerves, the latter being sympathetic and primarily vasomotor in nature.
Relations
Anterior Relations
The anterior Relations of 2 kidneys are very different.
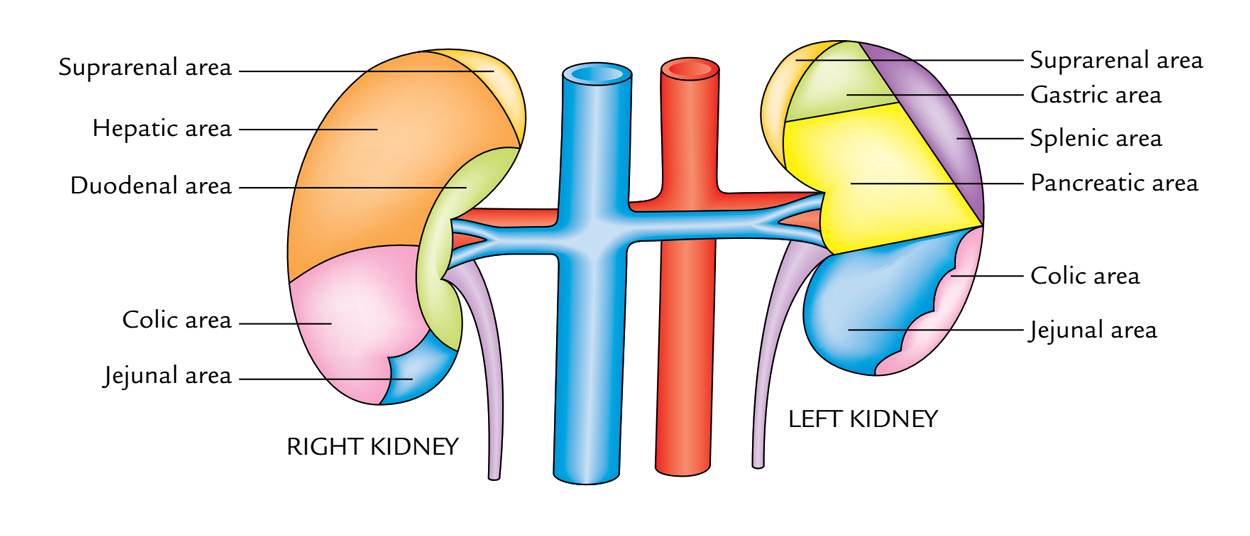
Kidneys: Anterior Relations
Anterior outermost layer of the right kidney:
- Right suprarenal gland.
- Right lobe of the liver.
- Second part of the duodenum.
- Hepatic (right colic) flexure.
- Jejunum.
Out of these, liver and jejunum are divided from the kidney by peritoneum.
Anterior surface of the left kidney:
- Left suprarenal gland.
- Spleen.
- Stomach.
- Pancreas and splenic vessels.
- Left colic flexure.
- Jejunum.
Out of these, stomach, spleen, and jejunum are divided from the kidney by peritoneum.
Posterior Relationships
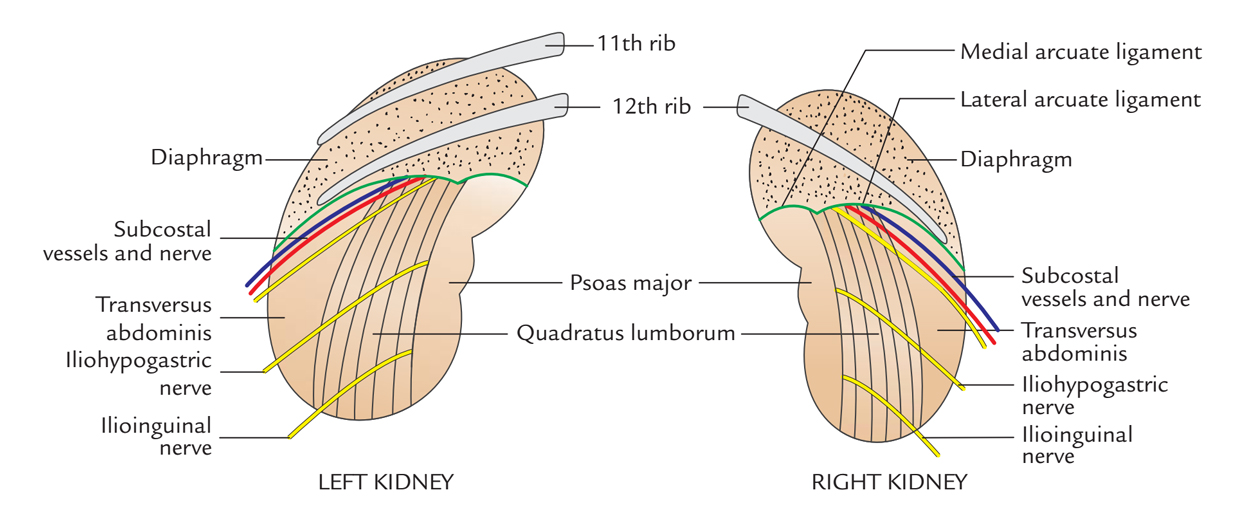
Kidneys: Posterior Relations
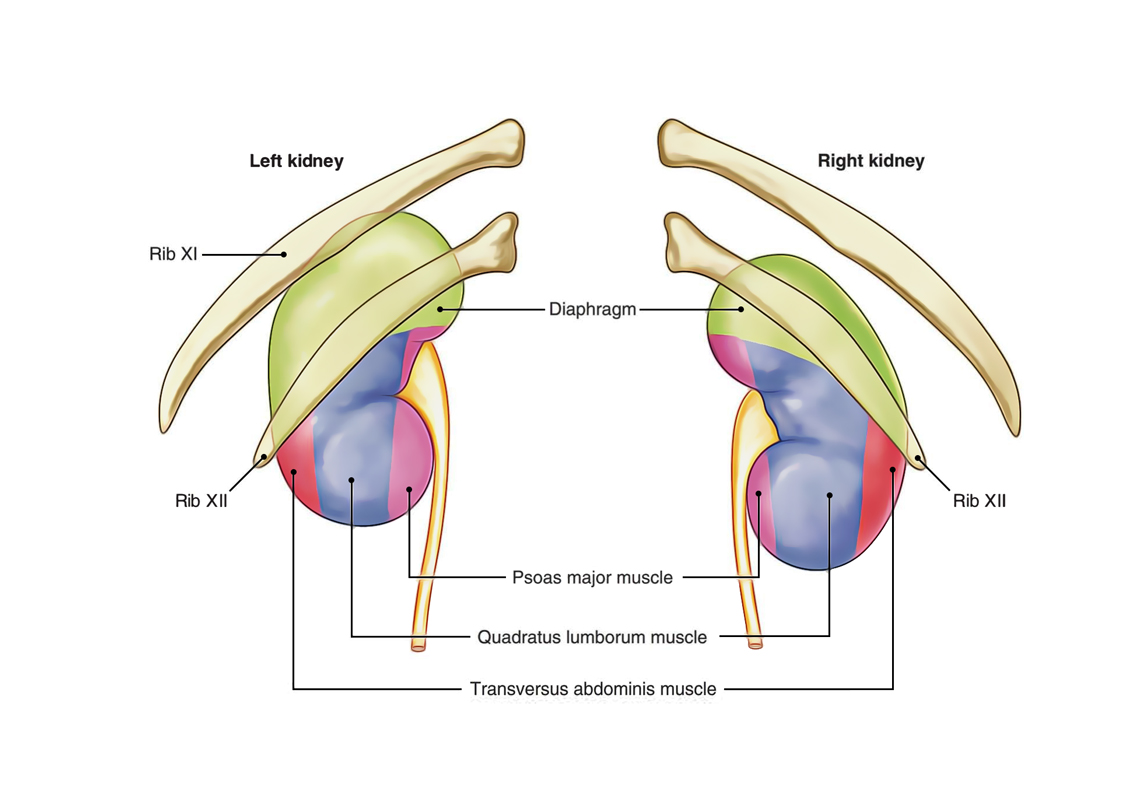
The posterior Relations of 2 kidneys are the same with the exception of that right kidney is related to 1 rib while left kidney is associated with 2 ribs:
- 4 muscles: Diaphragm, quadratus lumborum, psoas major, and transversus abdominis.
- 3 nerves: Subcostal (T12), iliohypogastric (L1), and ilioinguinal (L1). The subcostal nerve is escorted by the subcostal vessels.
- 1 or 2 ribs: The right kidney is associated with the 12th rib on the other hand the left kidney is associated with the 11th and 12th ribs.
The posterior Relations of both the kidneys are same with the exception of the right kidney is connected only to the 12th rib and the left kidney to the 11th and 12th ribs.
Capsules (Coverings) of Kidney
From inside outwards, the kidney is surrounded by 4 capsules/coverings as follows:
- Fibrous capsule (true capsule).
- Perirenal (perinephric) fat.
- Renal fascia (bogus capsule).
- Pararenal (paranephric) fat.
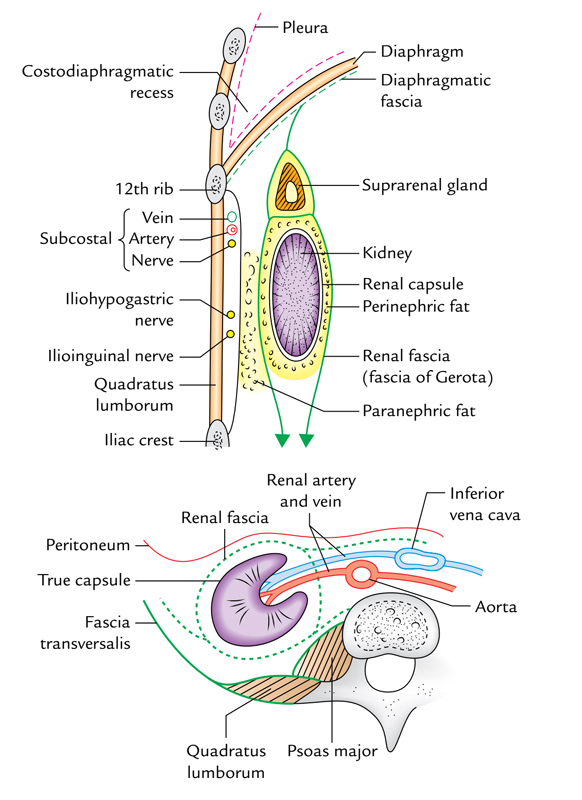
Kidneys: Capsules of Kidneys
Fibrous Capsule (True Capsule)
It’s a thin membrane which closely invests the kidney. It’s created by the condensation of fibrous connective tissue in the peripheral part of the organ. It’s easily stripped off from the face of the normal kidney. The capsule goes through the hilum to line the renal sinus and becomes constant with all the walls of calyces where they can be connected with the kidney. If the kidney is inflamed, this capsule becomes firmly adherent to the organ and can’t be stripped off.
Perirenal (Perinephric) Fat
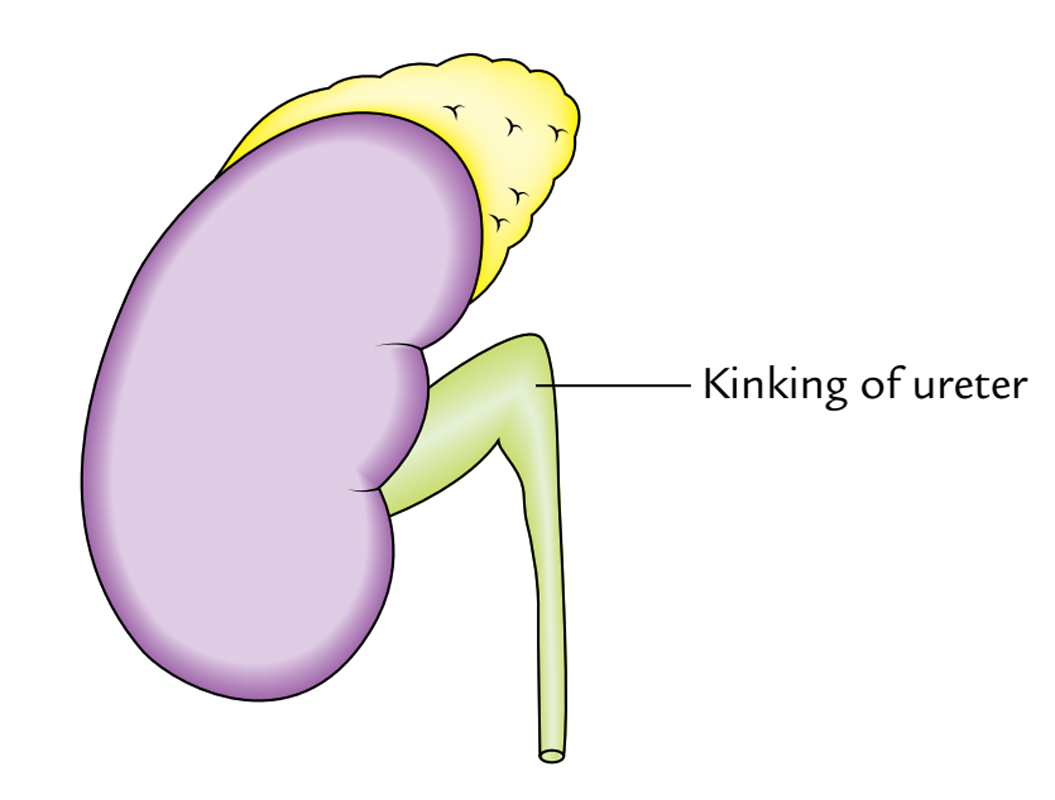
It’s a layer of adipose tissue, encompassing the fibrous capsule of the kidney. It fills the space inside the loosely fitting sheath of the renal fascia enclosing the kidney and suprarenal gland. This oily capsule is thickest at the edges of kidney and is prolonged via hilum into the renal sinus. In chronic debilitating diseases, the depletion of perinephric fat cancause downward displacement of the kidney, which may cause the kinking of the ureter.
Kidneys: Perirenal Fat
Renal Fascia (Fictitious Capsule/ Fascia of Gerota)
It’s a fibroareolar sheath, which surrounds the kidney and perirenal fat.
It contains the subsequent 2 layers:
- An ill defined anterior layer (fascia of Toldt).
- A well defined posterior layer (fascia of Zuckerkandl).
Extensions
- Superiorly, the 2 layers first enclose the suprarenal gland in another compartment and after that fuse with every other and become constant with the diaphragmatic fascia.
- Inferiorly, the 2 layers stay independent and enclose the ureter. The anterior layer is slowly lost in the extraperitoneal tissue of iliac fossa while the posterior layer mixes with the fascia iliaca.
- Laterally, the 2 layers blend steadfastly and become continuous with the fascia transversalis.
- Medially, the anterior layer enters in front of the kidney and renal vessels and unsites with all the connective tissue enclosing the aorta and inferior vena cava (IVC). The posterior layer enters on the other side of the kidney and is connected to fascia covering the quadratus lumborum and psoas major.
At the medial border of the kidney, the 2 layers are connected by a connective tissue septum being pierced by the renal vessels. Due to this connection (septum), perirenal effusion of the fluid doesn’t generally go across in the opposite perirenal space.
Pararenal (Paranephric) Fat
It’s a layer of fat being located outside the renal fascia. It contains substantial volume of fat being more plentiful posteriorlyand toward the lower pole of the kidney. It fills the paravertebral gutter and creates a pillow for the kidney.
Macroscopic Structure
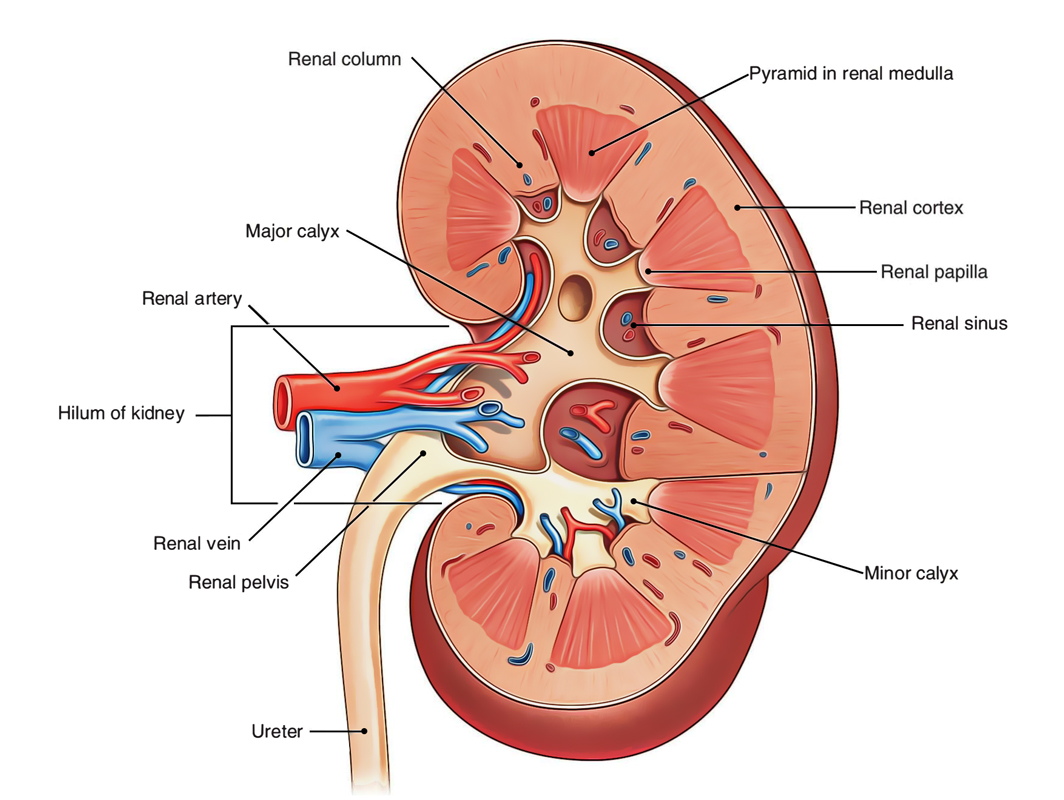
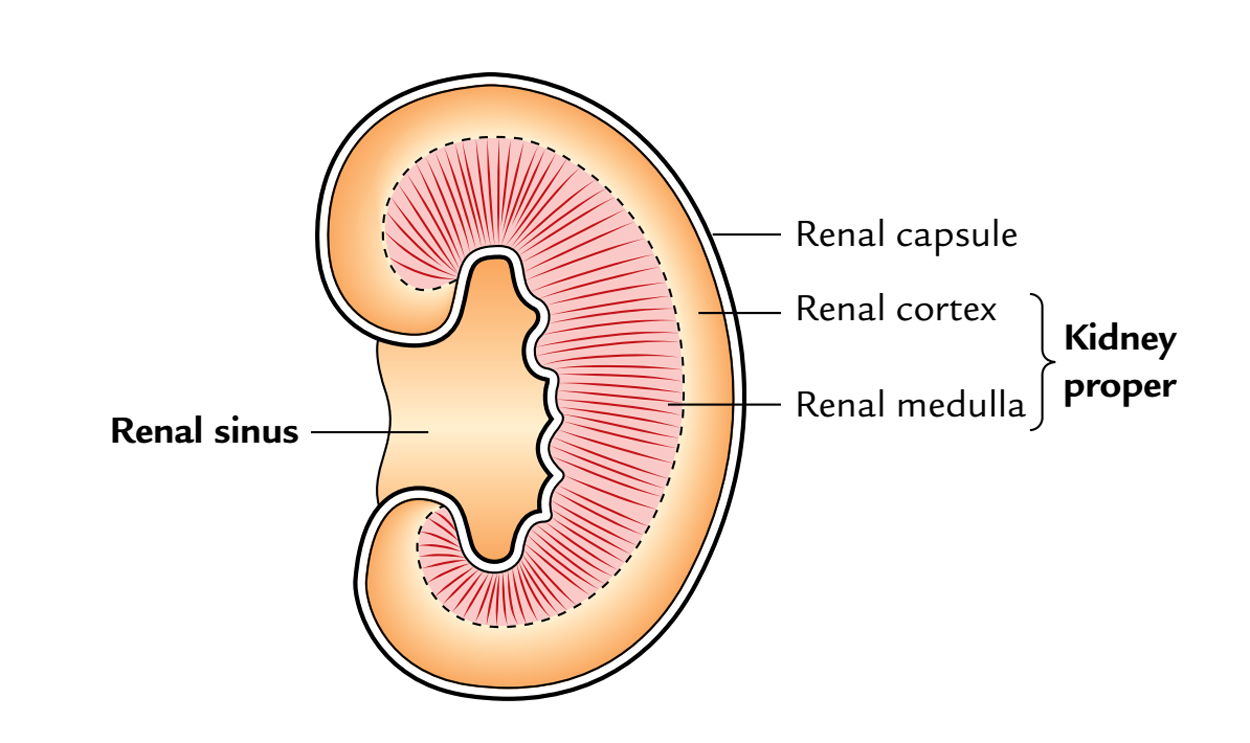
When the kidney is split longitudinally, it presents the kidney proper and the renal sinus.
Kidney Proper
Kidneys: Kidney Proper
- The naked eye evaluation of the kidney suitable presents an outer cortex and an inner medulla.
- The cortex lies just below the renal capsule and goes between the renal pyramids (vide infra) as renal Pillars (Pillars of Bertini). The cortex seems pale yellow with granular feel.
- The medulla consists of 5-11 dark conical masses named renal pyramids (pyramids of Malpighi). The apices of renal pyramids create nipple-like projections- the renal papillae which invaginate the minor calyces.
A renal pyramid together with its covering cortical tissue creates a lobe of the kidney.
Renal Sinus
It’s a cavity of significant size present inside the kidney. It takes up a large part of the inside of the kidney and opens at the medial border of the kidney as hilus.
Kidneys: Renal Sinus
It includes:
- Greater part of the renal pelvis, major and minor calyces.
- Renal vessels, lymphatics, and nerves.
- Fat.
The sinus is lined by the continuance of the true capsule of the kidney. Numerous nipple-like elevations (renal papillae) indent the wall of the sinus. The renal pelvis inside the sinus is split into 2 or 3 large branches, referred to as major calyces, which further splits to create 5-11 short branches referred to as minor calyces. Every small calyx enlarges as it approaches the wall of renal sinus, and its increased end is indented and moulded around the renal papilla. The gathering tubules inside the renal papilla open into the small calyx by perforating its wall and capsule lining the sinus. Therefore, the pelvis of ureter (upper funnel-shaped part of the ureter) is linked with the kidney tissue via calyces.
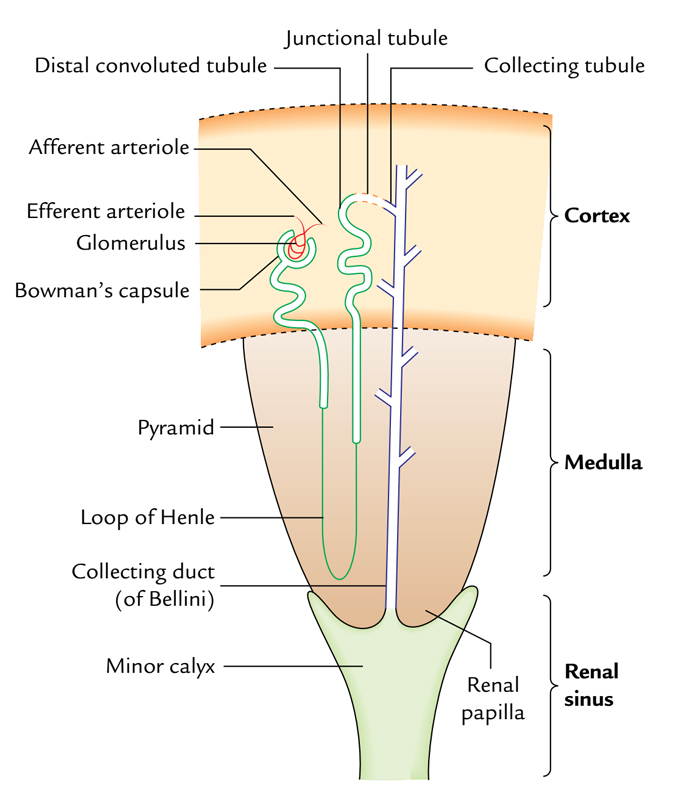
Microscopic Structure
Histologically, every kidney is composed of 1 to 3 millions of uriniferous tubules. Every uriniferous tubule is composed of 2 parts: nephron and gathering tubule.
Kidneys: Microscopic Structure
- The nephron is the structural and functional component of kidney. The number of nephrons in every kidney is all about 1-3 million. Every nephron is composed of a glomerulus and a tubule system. The glomerulus is a tuft of capillaries surrounded by Bowman’s capsule. The tubular system is composed of the proximal convoluted tubule, loop of Henle, and distal convoluted tubule.
- Every gathering tubule starts as a junctional (joining) tubule from the distal convoluted tubule. Many gathering tubules blend together to create gathering duct (duct of Bellini) which opens on the apex of renal papilla.
- The gathering tubules radiate from the renal pyramid into the cortical region to create radial striations referred to as medullary rays.
Clinical Significance
The absolute capacity of renal pelvis and major and minor calyces is about 8 ml. This fact would be to be held in mind while injecting radiopaque substance via ureter to outline these spaces because surplus of substance may split the ssites of continuity between the minor calyces and renal papillae.
Arterial Supply
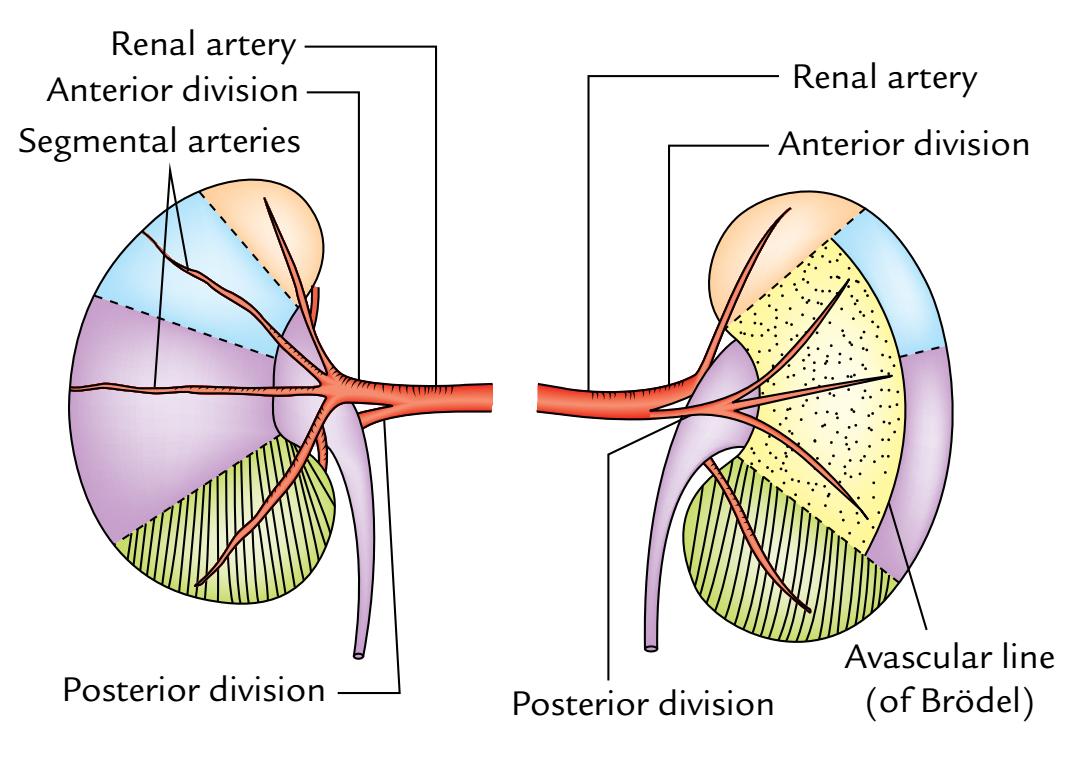
The kidneys are supplied by the renal arteries. Generally there’s 1 renal artery for every kidney, but in about 30% people accessory renal arteries are also seen. They generally originate from the aorta and goes into the kidney at the hilus or at 1 of its Poles, typically the lower post. The renal arteries have a blood flow in excess of 1 L/minute.
Renal Arteries
Kidneys: Renal Artery
The renal arteries originate directly from the abdominal aorta just below the origin of the superior mesenteric artery (i.e., at the level of intervertebral disc between L1 and L2).
The right renal artery enters to the right behind the inferior vena cava and right renal vein, while the left renal artery enters to the left behind the left renal vein.
- At or near the hilum of the kidney, every renal artery divides into anterior and posterior sections. The anterior section supplies apical, upper, middle, and lower sections, while posterior section supplies only posterior section. The branches supplying the segments are termed segmental arteries. The anterior segmental arteries are often bigger compared to the posterior.
- Every of these segmental arteries after supplying renal sinus breaks up into lobar branches.
- The lobar arteries break up into 2 or 3 interlobar arteries which go through renal Pillars between the pyramids.
- When an interlobar artery reaches the base of the affiliated pyramids, it breaks up dichotomously into the arcuate arteries.
- The arcuate arteries run parallel to the top layer of the kidney between the pyramids and the overlying cortex.
The renal arteries don’t anastomose with adjacent arcuate arteries but give branches which pass radiallytoward the top layer of the kidney that are referred to as interlobular arteries.
- The afferent arterioles from interlobular arteries pass to the capillaries of glomeruli, which in turn reunite to create efferent arterioles.
- The efferent arterioles split to create peritubular capillary plexus around the convoluted tubules.
- The capillaries drain in the interlobular veins and after that into interlobar veins, which run along the corresponding arteries.
- The interlobular veins drain into the arcuate veins which in turn drain into interlobar veins which go through the kidney tissue to the sinus in the place where they join to create the renal vein.
Vascular Sections
In accordance with Graves (1954), on the cornerstone of distribution of major branches of the renal artery every kidney is anatomically split into 5 vascular sections. Every section has its very own artery and between the sections there isn’t any anastomosis.
Aboce Diagram shows arterial segments of the kidney (left kidney in this figure): A, shows branches of the renal artery; B, C, and D show the segments as seen from anterior, lateral, and posterior aspects of the kidney, respectively
These sections are as follows:
- Apical is composed of the medial side and the anterior part of the superior post.
- Upper contains the rest of the upper post and the upper part of the anterior aspect.
- Middle contains lower part of the anterior aspect and is located between the upper and lower sections.
- Lower is composed of the whole of lower post.
- Posterior is composed of the whole of posterior aspect of the kidney between the apical and lower sections.
The segmental resection of kidney is possible if the disease is localized to 1 or more sections.
Venous Drainage
The venous blood from the kidneys is emptied by the renal veins (left and right). The left renal vein enters in front of the aorta immediately below the origin of the inferior mesenteric artery.
For all these sections, the Nomina Anatomica embraced a somewhat more descriptive terms, viz.,
- Superior.
- Anterosuperior.
- Anteroinferior.
- Inside.
- Posterior.
In the hilum/hilar area, the key renal artery divides into anterior and posterior sections. The anterior section supplies the apical, upper, middle, and lower sections, while the posterior section supplies the posterior section of the kidney.
- The junction between the regions supplied by the anterior and posterior sections of the renal artery is named Brodel’s line (a significant anatomical landmark). It’s on the posterior aspect of the kidney in the junction of medial 2 third and lateral one third. It’s a functional avascular plane between the posterior section medially and the upper and middle sections, thus suitable site for surgical incision to eliminate the renal stones (nephrolithotomy).
Lymphatic Drainage
The lymphatics from the kidney drain into the para-aortic lymph nodes at the level of origin of the renal arteries (L2).
Nerve Supply
Every kidney is supplied by the renal plexus of nerves which reach the kidney along the renal artery. The renal plexus contains both sympathetic and parasympathetic fibres. The sympathetic fibres are originated from T10 L1 spinal sections, and the parasympathetic fibres are originated from both vagus nerves.
Development
The above diagram shows development of the kidney:
A) Origin of the ureteric bud from mesonephric duct;
B) Point of union between the derivatives of the ureteric bud and metanephros (metanephric cap) indicated by an arrow.
- The kidney is composed of 2 parts- excretory and gathering. The excretory component comprising nephrons grow from the metanephros on the other hand thecollecting system being composed of gathering tubules, gathering ducts, small and major calyces, renal pelvis, and the ureter grows from the ureteric bud. The metanephros is originated from intermediate cell mass of the intraembryonic mesoderm while the ureteric bud is originated from the mesonephric duct.
- Initially, the kidney grows in the pelvis and is supplied by the internal iliac artery. Later it ascends up to its mature position gaining successively new arteries of supply from the common iliac and after that from the abdominal aorta. The elderly arteries degenerate as the brand new ones appear until the certain renal artery creates.
- The hilum of the kidney is at first anterior but the kidney rotates 90 ° medially causing the hilum to orient medially. The fetal kidney is lobulated.
Development of the Kidney
| Embryonic structures | Adult derivatives |
|---|---|
| Ureteric bud | 1. Collecting tubules 2. Collecting ducts 3. Minor calyces 4. Major calyces 5. Renal pelvis 6. Ureter |
| Metanephros | 1. Renal glomeruli 2. Bowman’s capsules 3. Proximal convoluted tubules 4. Loop of Henle 5. Distal convoluted tubules 6. Connecting tubules |
Clinical Significance
Congenital Anomalies
- Lobulated kidney: The determination of fetal lobulation in the adult kidney: It’s of no clinical importance.
- Aberrant artery: The tenacity of 1 of the fetal arteries is common (30% people), notably an artery from the aorta to the lower pole of the kidney.
- Congenital polycystic kidney: It’s is composed if the luminal continuity between the nephrons and gathering tubules don’t confirm. The glomeruli continue to excrete urine which collects in the tubules because of deficiency of outlet. Because of this tubules go through cystic enlargements (retention cysts).
- Horseshoe kidney (1 in 800): It happens because of fusion of the lower poles of the kidneys. The ureters pass anterior to the isthmus. The inferior mesenteric artery also enters anterior to the isthmus which restricts the rise of the horseshoe kidney.
- Renal agenesis (1 in 500): It happens when ureteric bud does not grow. Unilateral renal agenesis is comparatively common. A doctor shouldn’t presume that a patient has 2 kidneys. A surgeon must affirm this fact before contemplating nephrectomy.
Renal Pain
The renal pain is felt in the loin and frequently radiates downward and forwards into the groin. The disposition of pain changes from dull ache to acute spasmodic pain. The renal pain take place either because of stretching of the renal capsule or because of spasm of the smooth muscle in the renal pelvis. The afferent fibres pass successively via the renal plexus, lowest splanchnic nerve, sympathetic trunk, and goes into the T12 spinal section. The pain is often attributed along the subcostal nerve to the flank and anterior abdominal wall and along the ilioinguinal nerve (L1) into the groin.
Note: Tenderness in the kidney is aroused by applying pressure in the renal angle together with the thumb during inspiration. The renal angle is located between the lower border of 12th rib and the outer border of erector spinae.
Floating kidney (freedom of the kidney)
The kidney is kept in position by the perirenal fat and renal fascia. Nonetheless, every kidney moves up and down with respiration.
If the amount of perinephric fat is reduced, the freedom of the kidney becomes excessive (floating kidney) and may decrease the symptoms of the renal colic caused by the kinking of the ureter. A floating kidney can move up and down but not from the side to side inside the renal fascia.
Renal trauma
In spite of the fact that the kidneys are nicely shielded by the lower ribs, lumbar muscles and vertebral column, still a serious blunt injury of the abdomen may smash the kidney against the last 11th and/or 12th ribs, and the vertebral column. The penetrating injuries are often caused by stab or gunshot wounds. Since about 25% of the cardiac output goes through the kidneys, the critical renal injury can result in rapid blood loss.
Blood from the ruptured kidney or pus in a perirenal abscess first distends the renal fascia, then dribbles downward inside the fascial compartment and can get to the pelvis.
Transplantation of kidney
It’s done in chronic renal failure in selected cases. The donor kidney is set retroperitoneally in the iliac fossa with hilum parallel to the external iliac vessels. The renal artery is anastomosed end to end to the internal iliac artery and renal vein is anastomosed end to side to the external iliac vein. The ureter is implanted into the urinary bladder (ureterocystostomy).
Exposure of The Kidney from Behind
For posterior surgical approaches to the contents of the abdominal cavity, viz., kidney and ureter or the sympathetictrunk, 1 should understand the makeup of the posterior abdominal wall in the lumbar region. This is well appreciated by the anatomical vulnerability of the kidney from behind.
Loin: It’s the region on the rear of the trunk, bounded above by the 12th rib, below by the iliac crest, medially by the posterior median line, and laterally by flank.
Surface Mark of Kidney on the Back
It’s done inside parallelogram of Morris that is drawn in the following manner:
- First 2 horizontal lines are drawn 1 at the level of spine of T11 and other in the level of spine of L3.
- Afterward 2 vertical lines are drawn, 1 2.5 cm away and other 9 cm far from the posteromedian plane.
- The middle of hilum of the every kidney is located roughly at the lower border of L1.
Incisions
- Give median vertical incision extending from the spine of T11 to the spine of L2.
- Afterward make horizontal incisions extending from the upper and lower ends of the vertical incision.
Layers to be represented to reach the Kidney
The subsequent layers can be reflected 1 by one to be able to expose the kidney:
- Skin.
- Superficial fascia.
- Posterior layer of the thoraco-lumbar fascia with connected latissimus dorsi and serratus posterior inferior muscles.
- Erector spinae (sacrospinalis) muscles.
- Middle layer of the thoraco-lumbar fascia.
- Quadratus lumborum muscle.
- Anterior layer of the thoraco-lumbar fascia.
Renal Angle
- It’s an angle between the lower border of the 12th rib and the lateral border of erector spinae muscle.
- This angle becomes full following kidney enlargements and formation of perinephric abscess.
- It’s the site of tenderness in case of perinephric abscess. Renal pain is normally felt in this angle as a dull ache.
For better understanding of structures which are encountered during vulnerability of kidney, the pupils must understand about the thoraco-lumbar fascia.
Test Your Knowledge
kidney

 (59 votes, average: 4.54 out of 5)
(59 votes, average: 4.54 out of 5)