The lingual nerve is a sensory division belonging to the posterior branch of the mandibular division of the trigeminal nerve.
Lingual Nerve
Origin
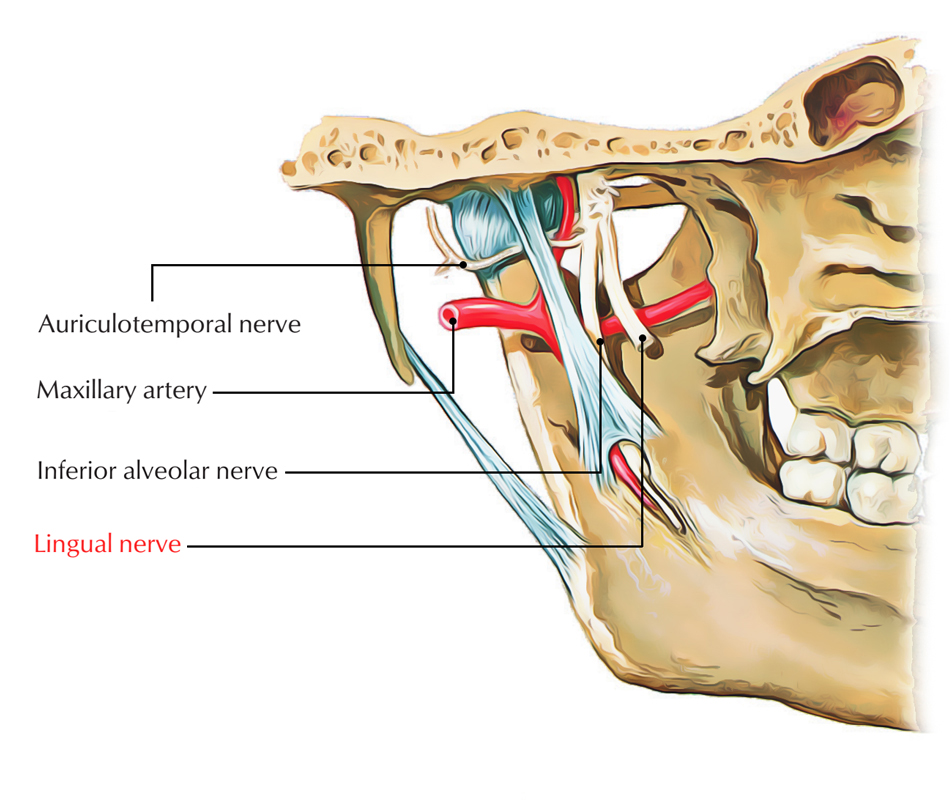
The lingual nerve arises via posterior division of the mandibular nerve and travels down in the middle of the ramus of the mandible as well as the medial pterygoid muscle.
Course and relations
It arises around 1 cm inferior towards the skull. It travels first among tensor palati and lateral pterygoid and then afterwards among lateral and medial pterygoid muscles.
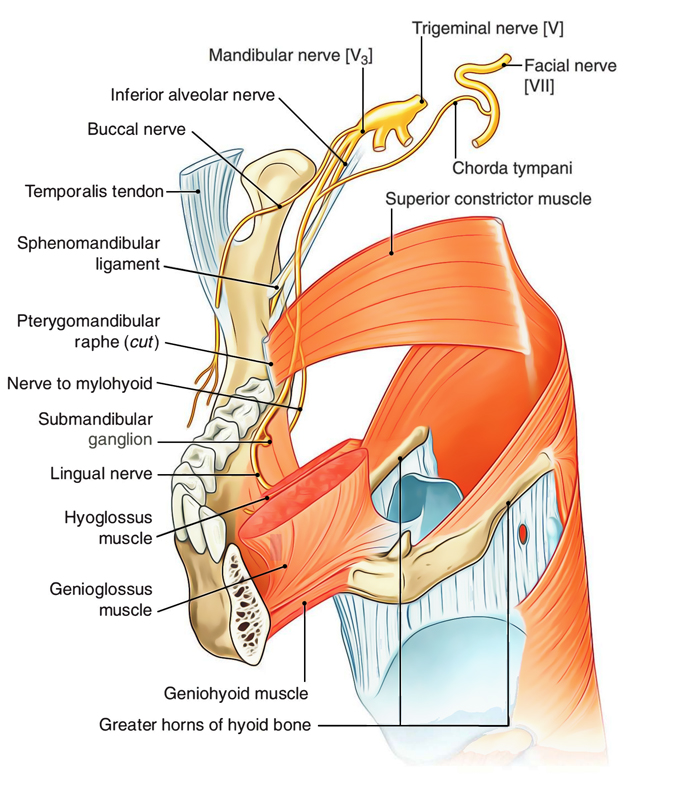
It combines with the chorda tympani nerve around 2 cm inferior towards the skull. After rising up at the lower margin of the lateral pterygoid, it first run inferior and anterior in the middle of the ramus of the mandible and medial pterygoid, comes in direct connection with the mandible where the bone is thinned, just above the posterior end of the mylohyoid line, in order to create a shallow hollow inferior and medial towards the last molar tooth.
Lingual Nerve – Course and Relations
This groove divides the attachments of pterygomandibular raphe superiorly and mylohyoid muscle inferiorly. On the superior surface of the mylohyoid it goes inside the mouth, and then it traverses the styloglossus in order to extend to the lateral side of the hyoglossus. Finally, it is located on the surface of the genioglossus. Here it coils around the submandibular duct and splits within its terminal divisions.
Branches
The lingual nerve produces the following two sets of branches:
- Branches of communication:
- Two or more which go towards submandibular ganglion.
- One or two branches which go inferiorly along the anterior margin of the hyoglossus in order to merge together with the hypoglossal nerve.
- Branches of distribution:
- A gingival branch towards the inner surface of the gum.
- Few branches towards the sublingual gland.
- Branches towards the anterior two-third portion of the tongue.
Function
From the mucous membrane of the anterior two-thirds of the tongue, the lingual nerve provides general somatic afferent innervation. It also conveys nerve fibers which are not a portion of the trigeminal nerve, like the chorda tympani nerve of the facial nerve, as well as parasympathetic and sympathetic fibers. The submandibular ganglion is overhung by the lingual nerve via two nerve strands.
Clinical Significance
Lingual Nerve Injury
Due to its anatomic position across space in the middle of the lingual part of the ascending ramus of the mandible as well as the tongue musculature posteriorly, lingual nerve injury can arise with mandibulotomy.
As many patients who require mandibulotomy due to cancer also need neck dissection, neck dissection can be performed first and in order to label the lingual nerve with a vessel loop which is meant for its careful preservation can be useful at the time of dissection of the floor of the mouth afterwards.
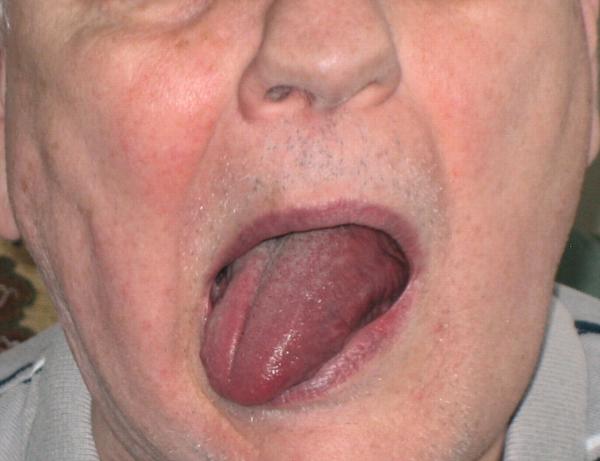
Burning paresthesia of the tongue may be created in a few patients after the repair of the floor of the mouth as a result of lingual nerve injury. The nerve is enveloped all over the Warthin duct of the submandibular gland within the floor of the mouth, and when the defect is being closed it can be injured with sutures. This paresthesia must be prevented because it is permanent.
Palsy of Lingual Nerve
Palsy of Lingual Nerve
Tongue numbness and a loss of the ability to taste are generally caused due to Palsy of the lingual nerve. By the compression of the endotracheal tube against tissue, injuries can occur with extensive surgical procedures of the head and neck. Generally, lingual nerve injury happens due to pressure against the mandible and the extending of the pterygoid muscles, which causes compression of the nerve. Sometimes, lingual nerve injury arises after placement in the prone position of the patient.

 (53 votes, average: 4.57 out of 5)
(53 votes, average: 4.57 out of 5)