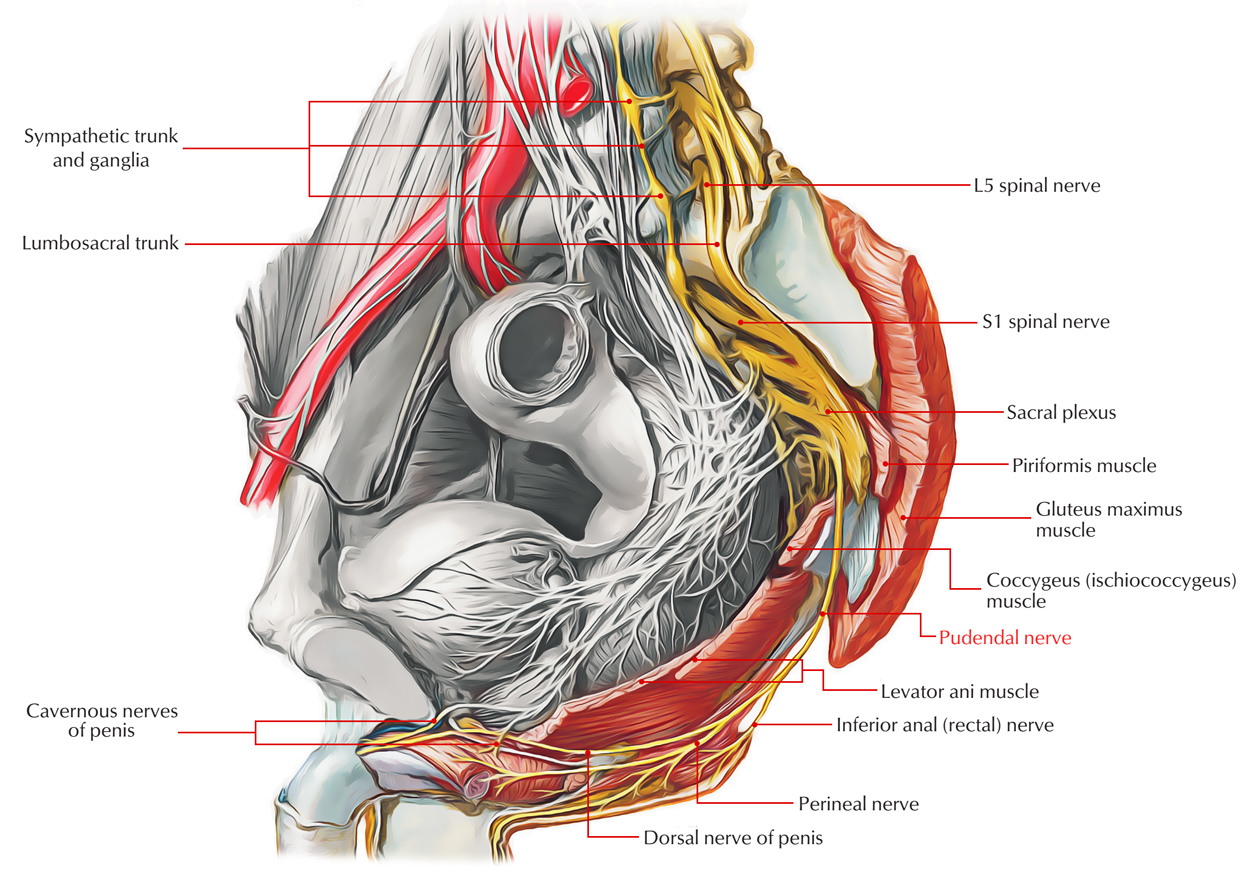
The Pudendal nerve exits the main pelvic cavity via the greater sciatic foramen and is a division of the sacral plexus. It goes into the perineum via the lesser sciatic foramen after a brief route within the gluteal zone of the lower limb. Within the pudendal canal the nerve then travels forward and innervates the external anal sphincter along with the muscles as well as skin of the perineum through its branches.
Pudendal Nerve
Branches
- Inferior rectal nerve: This travels medially across the ischiorectal fossa and innervates the mucous membrane of the lower half of the anal canal, the perianal skin, along with the external anal sphincter.
- Dorsal nerve of the penis (or clitoris): This is circulated towards the penis (or clitoris).
- Perineal nerve: This innervates the muscles inside the urogenital triangle along with the skin at the posterior side of the scrotum (or labia majora).
Insertion
- The pudendal nerve enters the gluteal zone via the greater sciatic foramen inferior towards the piriformis muscle and medial towards the sciatic nerve. It overpasses the sacrospinous ligament and directly travels through the lesser sciatic foramen in order to enter the perineum.
- The path of the pudendal nerve within the gluteal zone is short and the nerve is often hidden by overlapping upper boundary of the sacrotubcrous ligament.
- The pudendal nerve is the main somatic nerve of the perineum and also possesses no branches within the gluteal zone.
Course
- The pudendal nerve travels among the piriformis muscle as well as coccygeus (ischiococcygeus) muscles and also exits the lower portion of the greater sciatic foramen in the pelvis.
- It bridges the lateral part of the sacrospinous ligament and returns to the pelvis via the lesser sciatic foramen.
- After returning to the pelvis, together with the internal pudendal blood vessels it goes along with the internal pudendal artery as well as internal pudendal vein upwards and forwards around the lateral wall of the ischiorectal fossa, being held in a covering of the obturator fascia called the pudendal canal.
- Within the pudendal canal, the nerve splits into sections, first producing the inferior rectal nerve, after that the perineal nerve, just before proceeding as the dorsal nerve of the penis (in males) or the dorsal nerve of the clitoris (in females).
Functions
- The pudendal nerve possesses both motor as well as sensory functionalities. It does not have parasympathetic fibers, but does have sympathetic fibers.
- The pudendal nerve innervates the penis in males as well as the clitoris in females, via the sections dorsal nerve of penis along with dorsal nerve of clitoris.
- Through the posterior scrotal nerves (males) or posterior labial nerves (females) the posterior scrotum in males as well as the labia in females is also supplied.
- Branches also innervate the anal canal.
- By innervating the penis and the clitoris, the pudendal nerve causes the afferent part of penile erection as well as clitoral erection
- It also causes ejaculation
- Branches also stimulate muscles of the perineum along with pelvic floor; the bulbospongiosus and ischiocavernosus muscles, the levator ani muscle (consisting of the Iliococcygeus, pubococcygeus, puborectalis and also either pubovaginalis in females or puboprostaticus in males), the external anal sphincter (through the inferior anal branch) together with male or female external urethral sphincter.
- As it serves to stimulate the external urethral sphincter it causes the tone of the sphincter, moderated through acetylcholine discharge.
- This means that throughout times of enhanced acetylcholine discharge the skeletal muscle within the external urethral sphincter constricts, creating urinary retention.
- Compared to the internal sphincter muscle, the external sphincter is built from skeletal muscle; as a result it is within voluntary control of the somatic nervous system. While in times of reduced acetylcholine discharge the skeletal muscle inside the external urethral sphincter loosens, enabling emptying of the bladder.
Clinical Significance
Pudendal nerve blockage is another type of pudendal neuralgia. This disorder creates phantom pain (pain associated with an area which isn’t really part of the body) in the lower zones of the pelvis, penis and scrotum, vulva, anus, and perineum. People detected with pudendal nerve blockage have explained pain when taking a seat. This pain reduces when standing up or eliminating pressure. This disorder may be diagnosed in two ways:
Pudendal Motor Latency Examination
Doctors can carry out a pudendal nerve motor latency examination to decide if there is nerve damage. This examination determines the motor functionality of the nerve. If pudendal neuralgia is present, this examination will give doctors evidence.
Pudendal Block Examination
Doctors carry out this examination when they presume a pudendal nerve blockage. Doctors will use an anesthetic in order to desensitize the pudendal nerve. If the symptoms are eliminated, then pudendal nerve blockage is present.

 (54 votes, average: 4.89 out of 5)
(54 votes, average: 4.89 out of 5)