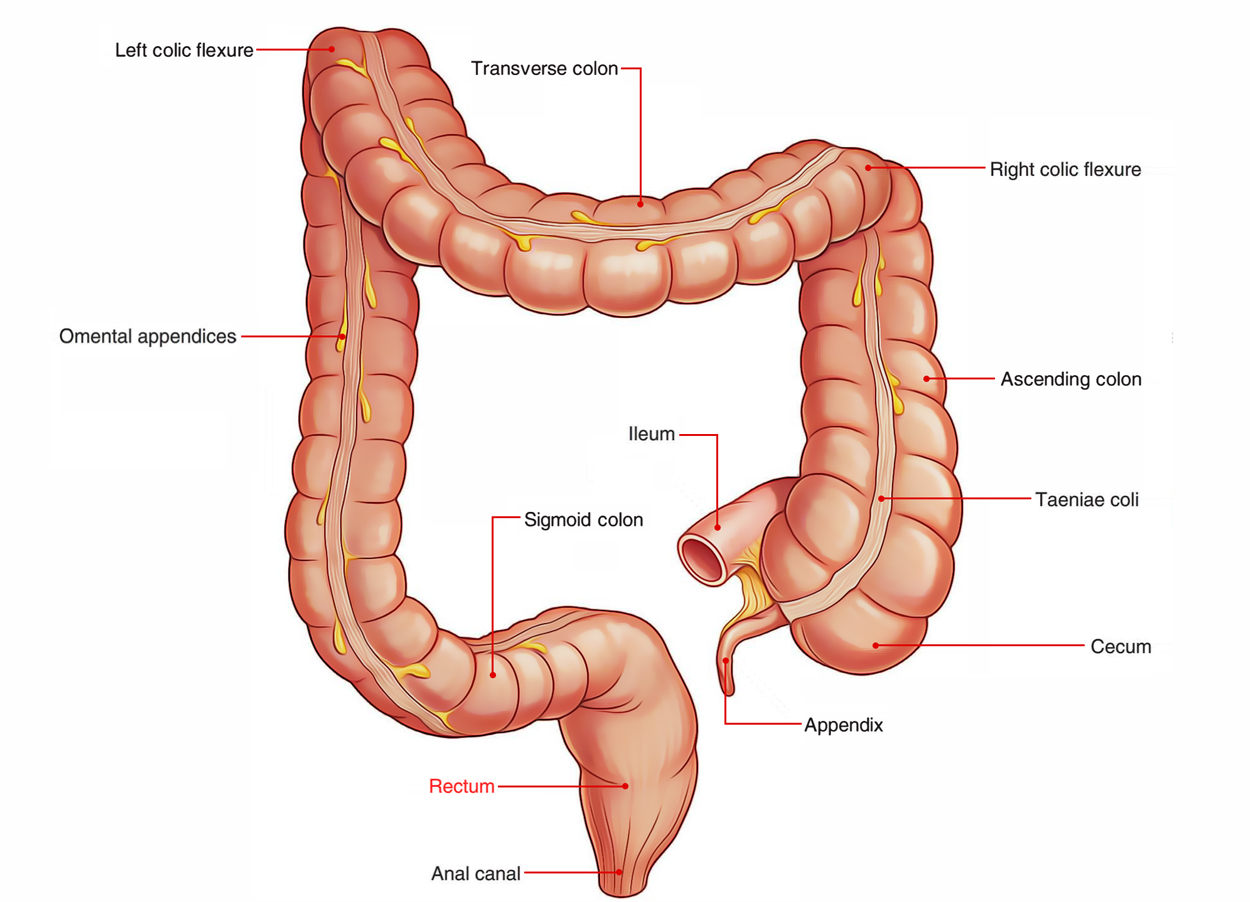
The Rectum is the distal part of the large intestine between the sigmoid colon and the anal canal. In Latin, the word “rectum” means straight; but the rectum is straight in quadrupeds and not in men. In spite of the fact that the rectum is a part of the large intestine, it’s devoid of taenia coli, sacculations and appendices epiploicae- the cardinal features of the large intestine.
The distension of the rectum begins the urge to defecate.
Rectum
Location
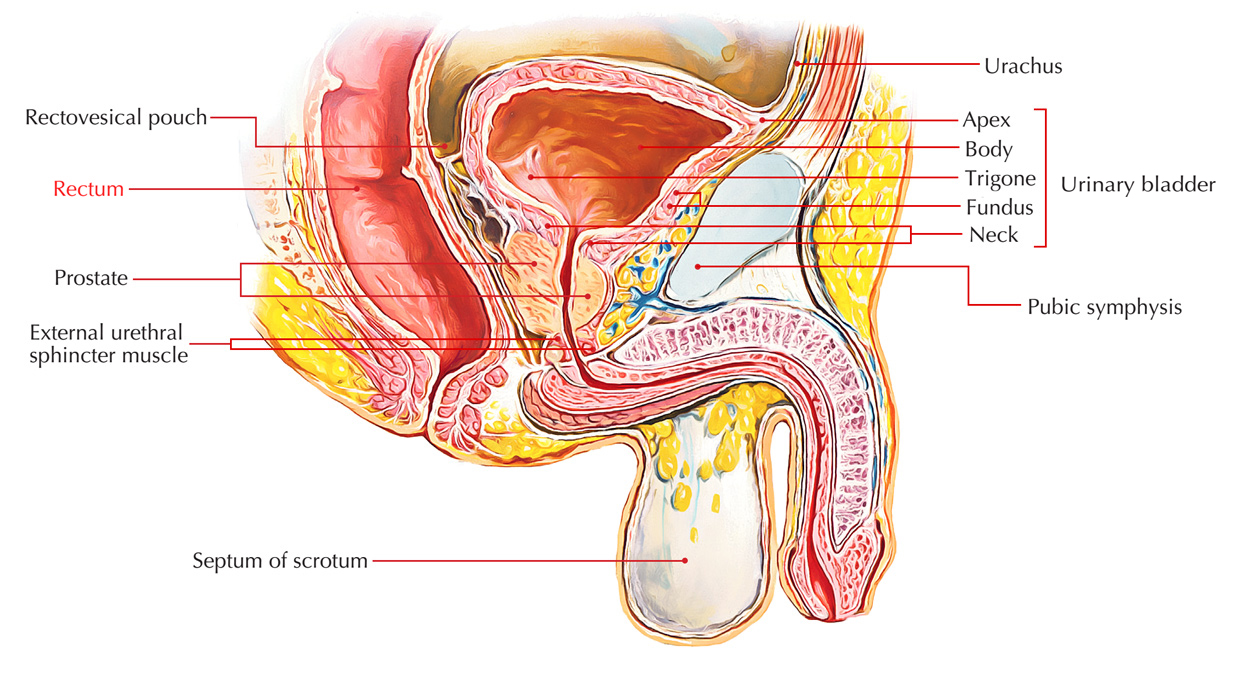
Rectum is situated in the posterior part of the lesser pelvis in front of the lower 3 sections of the sacrum and the coccyx and behind the urinary bladder in the male and uterus in the female.
Rectum: Location
Physiology
The rectum too can absorb water from faeces, in fact, it will wring faeces dry if they stay in the rectum too long. So if the “call to stool” is ignored for any length of time faeces can become stony hard and difficult, even painful, to pass.
This form of constipation is often thought of as a fault of the bowel or diet, but it isn’t. It’s simply due to not emptying the rectum soon enough. And it can be cured by heeding the call to stool as soon as you’re aware of it, even though the pressure to ignore it and do something else is strong. Laxatives aren’t necessary to cure this type of constipation, only retraining yourself to heed what your bowel is telling you to do. If you don’t, your bowel won’t bother to send you the signal and your “constipation” will worsen.
Measurements
The rectum is 5 inches (12 cm) long. The diameter of the rectum isn’t uniform throughout. In the upper part, the rectum is 4cm as that of the sigmoid colon. In the lower part, rectum creates a dilatation referred to as rectal ampulla. When empty the anterior and posterior walls of the rectum are in contact and cross section of the rectum presents lumen in the create of a transverse slit.
Extent And Course
The rectum starts as a continuation of the sigmoid colonin front of the 3rd sacral vertebra and becomes continuous with the anal canal about 2- 3 cm in front and a little belowthe tip of the coccyx. The rectosigmoid junction is indicatedby the lower end of the sigmoid mesocolon.
From its start in front of S3 vertebra, first rectum runs downward and backwards, then vertically downward, and.
Eventually downward and forward. About 2.5 cm in front and a little below the tip of coccyx, rectum suddenly turns downward and backward to become constant with the anal canal. The anorectal junction corresponds with the apex of prostate inmale.
To summarize the direction of the course is as under:
- In the upper third- rectum is pointed downward and backward.
- In the middle third- rectum is directed vertically downward.
- In the lower third- rectum is pointed downward and forward.
Curvatures (Flexures of the Rectum)
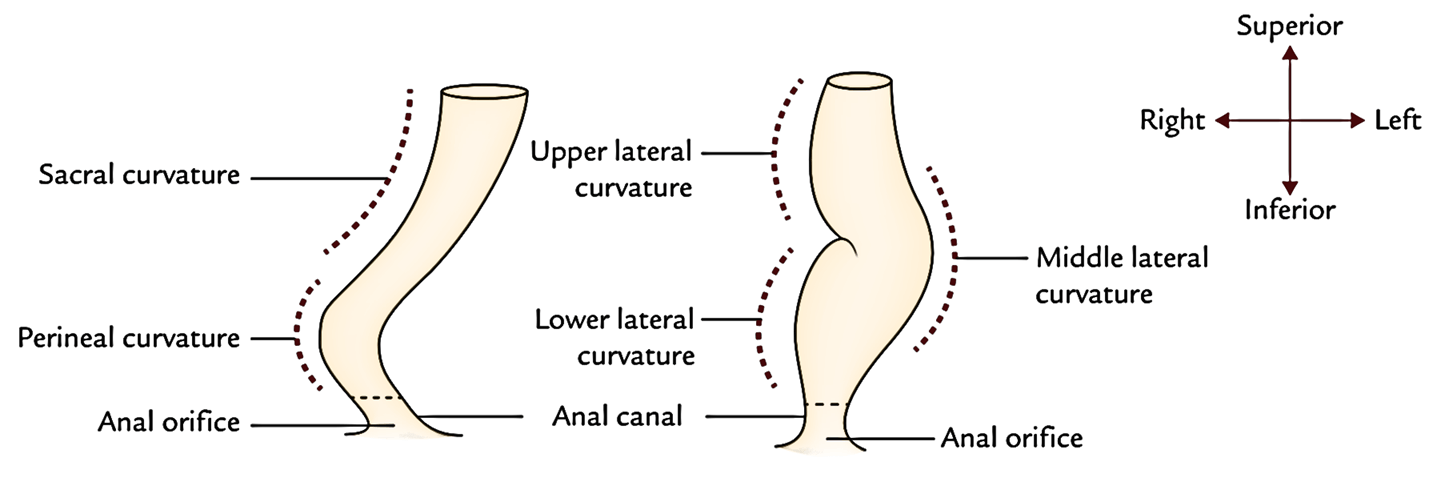
The rectum presents curvatures in both anteroposterior andlateral planes.
Rectum: Curvatures
Anteroposterior Curvatures
All these are 2 in number, an upper sacral curvature and alower perineal curvature.
- Sacral curvature corresponds to the concavity of the sacrum and coccyx.
- Perineal curvature corresponds to the forward bending of the anorectal junction. It’s preserved by the puborectal sling originated from the levator ani.
Rectum: Anteroposterior Curvatures
Lateral Curvatures
These are 3 in number and present in the create of twoconvexities to the right side and 1 convexity to the left side.
- Upper lateral curve is convex to the right at the junction of S3, S4 vertebrae.
- Middle lateral curvature is convex to the left at the sacrococcygeal junction. It’s the most notable curvature.
- Lower lateral curvature is convex to the right at the level of tip of the coccyx.
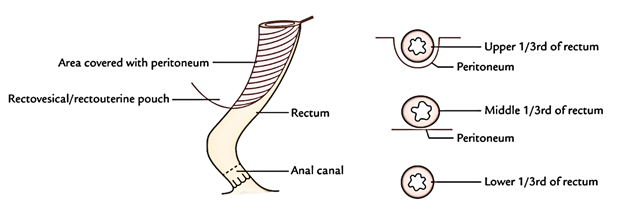
Peritoneal relations of the Rectum
Rectum: Peritoneal Relation
The peritoneal relationships of the rectum are as under:
- Upper one third of the rectum is covered with the peritoneum on the front and sides.
- Middle one third of the rectum is covered with the peritoneum only on the front.
- Lower 1-third of the rectum (ampulla) isn’t covered by the peritoneum at all.
The ampulla of rectum is located below the level of rectovesical pouch in the male and rectouterine pouch in the female.
Relations
Anterior Relations
Anterior relationships of the prectum in male and female.
| Relations | ||
|---|---|---|
| Portion of rectum | In male | In female |
| Upper two-third of rectum(peritoneal) | Rectovesical pouch and coils of the small intestine andsigmoid colon within it | Rectouterine pouch and coils of the smallintestine and sigmoid colon within it |
| Lower one-third of rectum/ ampulla (non-peritoneal) | 1. Base of the urinary bladder 2. Ureters (terminal parts) 3. Seminal vesicles 4. Ampullae of vas deferensProstate | Lower one-third of rectum/ ampulla (non-peritoneal) |
| (All these structures are separated from the rectum by the well-defined rectovesical fascia of Denonvilliers) | Vagina (lower part) (It is separated fromrectum by an ill-defined rectovaginal fascia) | (All these structures are separated from the rectum by the well-defined rectovesical fascia of Denonvilliers) |
Posterior Relationships
Posterior Relations of the rectum in male and female.
Rectum: Posterior Relationship
| Posterior relations | |
|---|---|
| In the midline | On each side of midline |
| Lower three pieces of sacrum | Piriformis |
| Coccyx | Coccygeus |
| Anococcygeal raphe | Levator ani |
| Ganglion impar | Sympathetic chains |
| Median sacral vessels | Anterior primary rami of S3, S4, S5, and coccygeal nerve (Co1) |
| Superior rectal artery (opposite S3 vertebra only) | Pelvic splanchnic nerves |
| Fascia of Waldeyer | Lateral sacral vessels |
Lateral Relations
- Upper part of rectum is related to pararectal fossae consisting of coils of small intestine and sigmoid colon.
- Lower part of rectum is associated with levator ani muscles which closely surround it and supply support.
Inside of the Rectum
- The inner part of the rectum presents 2 types of mucosalfolds- temporary and long-lasting.
- Temporary folds are mainly longitudinal and seen in thelower part of the rectum. They evaporate when rectum distends.
- Long-Term folds (or Houston’s valves) are semilunar (crescentic) transverse folds situated against the concavities of the lateral curvatures of the rectum. They’re created by the reduplication of the mucous membrane consisting of submucous tissue and thickening of circular smooth muscle of the rectal wall.
They can be long-term and become more notable when the rectum is distended. Based on Houston, they’re 4 in number and are numbered from above downward as follows:
- First fold (or upper fold) is located near the upper end close to the rectosigmoid junction. It projects from the left or right wall.
- Second fold is located about 1 inch (2.5 cm) above the third fold and projects from the left rectal wall along the concavity of upper lateral curvature.
- Third valve is the largest, most continuous, and most essential. It projects from the anterior and right wall of the rectum along the concavity of middle lateral curvature. It is located at the level of upper end of ampulla.
- Fourth valve projects from the left wall of the rectum along the concavity of lower lateral curvature. It is located about 2.5 cm below the third valve.
The transverse folds of the rectum (rectal valves) supply support to hold the faeces and stop the excessive distension of the rectal ampulla. They can be viewed per anum with the help of a speculum.
Clinical Significance
The semilunar transverse folds of the rectum (rectal valves), especially the 3rd valve, causes hindrance in passing an instrument from the anus. Thus, the canula for rectal washing/sigmoidoscope is generally passed in the left lateral position of the patient to prevent injury to Houston’s third valve and give a wide berth to unnecessary suffering to the patient.
Arterial Supply
Rectum: Arterial Supply
The rectum is supplied by the following arteries:
- Superior rectal artery (main artery of the rectum), a continuance of the inferior mesentery artery.
- Middle rectal arteries (2 in number). Every is a branch from the anterior section of the internal iliac artery.
- Inferior rectal arteries (2 in number). Every is a branch of internal pudendal artery.
- Median sacral artery, a branch of the abdominal aorta.
Superior Rectal Artery
It’s the primary/main artery of the rectum and supplies whole mucous membrane up to the anal valves, and the musculature of the upper part of the rectum. It’s the continuance of the inferior mesenteric artery (at the pelvic brim) and reaches the rear of the rectosigmoid junction opposite the S3 vertebra, where it splits into left and right branches. The right branch farther divides into anterior and posterior branches. The branches of both sides subdivide into smaller branches, which pierce the rectal wall and create looped anastomoses in the submucous layer of the lower part of the rectum. From this plexus, straight vessels descend in the anal Pillars and anastomoses with the branches of the inferior rectal artery at the pectinate line.
Middle Rectal Arteries
The middle rectal artery is a branch of anterior section of the internal iliac artery and enters downward and medially via the lateral ligament of the rectum and supplies the lower part of the rectum. The middle rectal arteries are unimportant because they supply only the superficial layers of the rectum.
Inferior Rectal Arteries
The inferior rectal artery is a branch of the internal pudendal artery. It enters across the ischiorectal fossa to supply the perianal skin, anal sphincters, and anastomoses with the branches of the superior rectal artery at the pectinate line.
Median Sacral Artery
It’s a small branch, which originates from the posterior aspect of the aorta near its lower end. It descends in the median plane to supply the posterior wall of the anorectal junction.
Venous Drainage
Rectum: Venous Drainage
The venous blood from the rectum is emptied by the following veins:
- Superior rectal vein.
- Middle rectal veins (2 in number).
- Inferior rectal veins (2 in number).
The rectal veins originate from internal and external venous plexuses of the rectum and anal canal.
The internal venous plexus is within the submucous coat and encircles the anal canal above Hilton’s line. The external venous plexus is present between the perianal skin and the subcutaneous part of the external anal sphincter. It encircles the anus. The internal and external venous plexuses communicate with every other.
Therefore, the lower part of the rectum and the anal canal are encircled by a venous plexus termed annulus hemorrhoidalis.
Superior Rectal Veins
The tributaries of the vein start in the anal canal from the internal rectal venous plexus in the create of 6 veins. They pass upward via the anal Pillars and submucous layer of the rectum, and unify to create the superior rectal vein which pierces the muscular layer of posterior rectal wall about 3 inches (7.5 cm) above the anus. The superior rectal vein continues upward as the inferior mesenteric vein which empties into the splenic vein (portal system).
Middle Rectal Veins
These veins originate 1 on every side from the middle of venous plexus, pass along the lateral pelvic wall, and drain into the internal iliac vein (systemic vein).
Inferior Rectal Veins
These veins originate from the lower part of the plexus. Every vein stretches across the ischiorectal fossa and drains into the internal pudendal vein on the corresponding side.
The superior rectal vein, a tributary of portal vein creates anastomosis with middle and inferior rectal veins the tributary of inferior vena cava in the level of mid-anal canal (1 of the essential ssites of portocaval anastomosis).
Lymphatic Drainage
Lymphatics from the upper half accompany the superior rectal vessels and drain into the inferior mesenteric nodes. Some of these vessels are intercepted by the pararectal lymph nodes situated on every side of the rectosigmoid junction.
Rectum: Lymphatic Drainage
Lymphatics from the lower half accompany the middle rectal vessels and drain into the internal iliac nodes.
Clinical Significance
The lymphatics of the rectum are largely arranged longitudinally in sharp contrast to the lymphatics of the majority of the small and large intestines, where they can be ordered transversely around the gut.
So, when the carcinoma of the rectum disperses along lymphatics it will not cause rectal obstruction unlike the remainder of the gut.
Nerve Supply
The rectum is supplied by both sympathetic and parasympathetic fibres. The sympathetic fibres are originated from L1, L2 sections of the spinal cord and parasympathetic fibres from S2, S3, S4 sections of the spinal cord.
Supports of the Rectum
The rectum is kept in position and prevented from prolapse by these structures:
- Pelvic diaphragm: It’s created by the levator ani muscles. The puborectalis sling of the diaphragm encompasses the anorectal junction and keeps the anorectal flexure.
- Fascia of Waldeyer: It’s a connective tissue supporting the rectum. It goes from the lower part of rectal ampulla to the sacrum and coccyx. It includes perirectal fat, lymph nodes, lymphatics, and superior rectal vessels.
- Lateral ligaments of the rectum: All these are fibrous groups created by the condensation of pelvic fascia 1 on every side of the rectum. They connect the rectum to the posterolateral walls of the lesser pelvis and include the middle rectal vessels.
- Rectovesical fascia of Denonvilliers.
- Reflection of pelvic fascia from parietal to visceral layers around the rectum.
- Pelvirectal and ischiorectal fat serve as a loose packing material around the rectum and anal canal.
- Pelvic peritoneum and associated vascular pedicles.
- Perineal body.
Clinical Significance
Prolapse of Rectum
It’s the protrusion of the rectum via the anus. The prolapse might be incomplete or whole.
- Incomplete prolapse (mucous prolapse): It’s the protrusion of rectal mucosa via the anus and takes place because of excessive straining during defecation. This is because of imperfect support of the rectal mucosa by the submucosa.
- Entire prolapse (procidentia): In this state, entire thickness of the rectal wall protrudes via the anus. The causative variables are laxity of the pelvic diaphragm, excessively deep rectovesical or rectouterine pouch and insufficient fixation of the rectum in its presacral bed.
Medically, it presents as (a) protrusion of the bowel via the anus, (b) mucous discharge and bleeding, (c) pain, and (d) anal incontinence (because of stretching of internal and external anal sphincters).


 (62 votes, average: 4.45 out of 5)
(62 votes, average: 4.45 out of 5)