The soft tissues covering the vault of skull are called scalp. External occipital protuberance and nuchal lines are the source from where the scalp extends to the supraorbital margins.”
Extent
It goes anteriorly up to the eyebrows (superciliary arches), laterally on every side up to superior temporal line and posteriorly up to the superior nuchal lines. According to some authorities, scalp stretches laterally on every side, up to the zygomatic arch.
Layers
Scalp
The scalp is composed of 5 layers. From superficial to deep these are as follows:
- Skin.
- Connective tissue (superficial fascia).
- Aponeurosis (occipitofrontalis muscle and its aponeurosis).
- Free areolar tissue.
- Pericranium.
The sequence of the layers of scalp can be easily remembered by a perfect mnemonic SCALP derived by using initial letter of every layer.
Skin
The skin of scalp is thick and hairy with the exception of over the brow. It’s firmly adherent to epicranial aponeurosis by holese connective tissue of superficial fascia, as in palms and soles. Being hairy it includes maximum number of hair follicles and related sebaceous glands. Consequently, scalp is the commonest site of sebaceous cysts. It also includes numerous sweat glands. It is often estimated that there are about 1,20,000 hair on the scalp of an adult individual. About 20-100 hair are lost daily and replaced concomitantly. The baldness (loss of hair) primarily affects males and few aged females with high level of androgenic hormones within their blood.
Connective Tissue (Superficial Fascia)
The superficial fascia of the entire scalp is composed of holese fibrous connective tissue that securely binds the skin to the inherent occipitofrontalis and its aponeurosis. Fibrous septa break up this layer into numerous small pockets featuring lobules of fat. The blood vessels and nerves of the scalp are located in this layer. They go into it from below at the periphery. The walls of the vessels are adherent to the fibrous internet-work; for this reason when blood vessels are torn or cut during an injury, they are unable to retract and cause profuse bleeding. The bleeding, nonetheless, can be stopped by pressing against the underlying bone.
Aponeurosis
This layer is composed of occipitofrontalis muscle and its aponeurosis. The occipitofrontalis muscle includes 4 small abdomens: 2 frontal abdomens and 2 occipital midriffs. Since greater part of the layer is composed by aponeurosis, it is termed as aponeurotic layer. The aponeurosis of occipitofrontalis muscle is also termed epicranial aponeurosis or galea aponeurotica (Latin: galea = helmet). The wounds of the scalp don’t gape unless epicranial aponeurosis is cut transversely since the aponeurosis is under tension in the anteroposterior direction by the tone of occipitofrontalis muscle.
Loose Areolar Tissue
As the particular name suggests, this layer is made from loose areolar tissue. It acts as a natural plane of cleavage during craniotomy. This layer is traversed by emissary veins joining veins in the second layer of scalp with intracranial dural venous sinuses. Pericranium: The fifth layer of scalp is composed by the periosteum of bones of vault of skull named pericranium. It’s loosely connected to the bones and can be easily stripped, but at sutures it’s securely connected to sutural membrane, which in turn attaches it to the endocranium (the periosteum covering inner aspect of the skull bones).
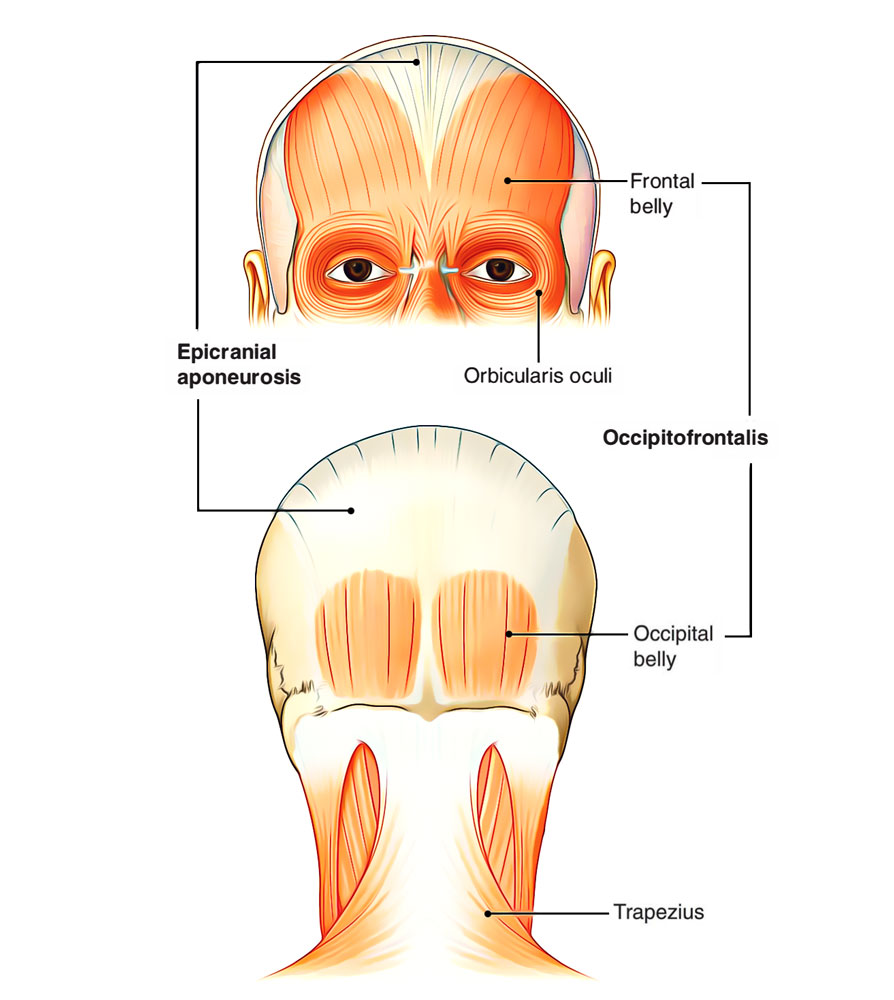
Occipitofrontalis Muscle
Occipitofrontalis Muscle
Origin and Insertion
The frontal midriffs originate from skin and subcutaneous tissue over the eyebrows and root of the nose, run backwards to be fit into epicranial aponeurosis in front of coronal suture. They’ve no bony connection of their own. The deeper fibres of frontal abdomen unite with procerus, corrugator supercilii and orbicularis oculi muscles. The front abdomens are longer, wider and partially united with every other along their medial edges. The occipital bellies originate from lateral two-third of the superior nuchal lines and go forwards to be added in the epicranial aponeurosis. The 2 occipital midriffs are small and divided from every other by a large gap. This gap is filled up by epicranial aponeurosis.
Nerve Supply
The occipital belly on every side is supplied by posterior auricular branch of facial nerve while the frontal abdomen is supplied by temporal branch of the facial nerve.
Activities
- Alternative contractions of frontal and occipital bellies move the scalp forwards and backwards over the vault of the skull.
- Acting from above, the contraction of frontal abdomens raises the eyebrows as in surprise.
- Acting from below, the contractions of frontal midriffs generate transverse wrinkles on the brow as in fright.
Clinical Significance
Surgical Layers of the Scalp
First 3 layers of the entire scalp, i.e., skin, connective tissue layer and aponeurotic layer are steadfastly stuck to every other and can not be divided from every other. These layers are referred to as surgical layers of the entire scalp and create the scalp appropriate. The layer of loose areolar tissue below the aponeurotic layer accounts for the complimentary mobility of the scalp suitable on the underlying bone. Further, it gives a simple plane of cleavage in injury and a plane where blood from severed blood vessels can distribute for a long distance. When the hairs are caught in machines, the scalp suitable is avulsed. The Red Indians of bygone days utilized to eliminate the scalp (appropriate) of their casualties as punishment. It’s in this plane that surgeons marshal scalp flaps.
Black Eye
The blood and fluid gathering in the layer of loose areolar tissue following a strike on head tracks freely under the scalp creating generalized swelling over the dome of the skull, but cannot enter either occipital or temple regions due to the bony attachments of the occipitofrontalis. The blood and fluid can, though, track forwards into the eyelids because occipitofrontalis has no bony connection anteriorly. This result in creation of hematoma few hours after a head injury or cranial surgery causing black discoloration of skin around the eyes, a condition named black eye.
It’s significant to notice that the commonest cause of black eye is localized violence, like fist fight causing sub-cutaneous extravasation of blood into the eyelids.
Dangerous Area of the Scalp
The layer of loose areolar tissue is named dangerous layer of scalp because blood and pus freely have a tendency to accumulate in this layer. If pus accumulates in this layer, the infection may go easily along emissary veins into the intracranial dural venous sinuses resulting in their thrombosis, which might be deadly. Safety valve hematoma, cephalhematoma and caput succedaneum. Fracture of cranial vault in kids may be related to the snapping of dura mater and pericranium. In such cases the blood from intracranial hemorrhage interacts with the subaponeurotic space of the entire scalp via the fracture lines. The signs of cerebral compaction don’t grow until the subaponeurotic space is completely full of blood. Because of this the collection of blood in the fourth layer is referred to as a safety valve hematoma. If cerebrospinal fluid accumulates in the subaponeurotic space, the state is named cephalhydrocele. Cephalhematoma is a subperiosteal collection of blood. Since the periosteum of skull loosely covers the bones of skull with the exception of at the sutural lines where it’s securely connected to the sutural membranes, the hematoma is bound by suture lines and assumes the shape of associated bones. It’s solid and its borders are well defined. A cephalhematoma is often seen in the parietal region. Caput succedaneum is a subcutaneous edema over the presenting part of the head at delivery. It happens during the passage of head via the beginning canal because of hindrance of the venous return. It’s the most frequently encountered create of beginning trauma of the entire scalp and generally takes place over the occiput and crosses the suture lines. The affected parts of the scalp feel soft and margins are partially defined. Usually the edema subsides, in a couple of days.
Nerve Supply
Nerve Supply of Scalp
Sensory Supply of The Scalp
Scalp: Sensory Supply
The scalp on every side of the midline is supplied by 8 sensory nerves: 4 in front of the auricle and 4 supporting the auricle. The nerves in front of the auricle are originated from trigeminal nerve, on the other hand those behind the auricle are originated from the second and third cervical nerves. Sensory nerves of the scalp
| In front of the auricle (from before backwards) | Behind the auricle (from before backwards) |
|---|---|
| Supratrochlear, a branch of frontal nerve from ophthalmic division of trigeminal nerve | Great auricular, derived from ventral rami of 2nd and 3rd cervical nerves |
| Supraorbital, a branch of fontal nerve from ophthalmic division of trigeminal nerve | Lesser occipital, derived from ventral ramus of 2nd cervical nerve |
| Zygomaticotemporal, a branch of zygomatic nerve from maxillary division of trigeminal nerve | Greater occipital, derived from dorsal ramus of 2nd cervical nerve |
| Auriculotemporal, a branch of mandibular division of trigeminal nerve | Third occipital, derived from dorsal ramus of 3rd cervical nerve |
Motor Supply of the Scalp
The scalp on every side of the midline is supplied by 2 motor nerves: 1 in front of the ear and 1 behind the ear; both these nerves are originated from the facial nerve.
Motor Supply of Scalp
Nerve in front of the ear is temporal branch of the facial nerve. It supplies frontal abdomen of occipitofrontalis muscle. Nerve supporting the ear is the posterior auricular branch of the facial nerve. It supplies occipital belly of occipito-frontalis muscle.
Arterial Supply
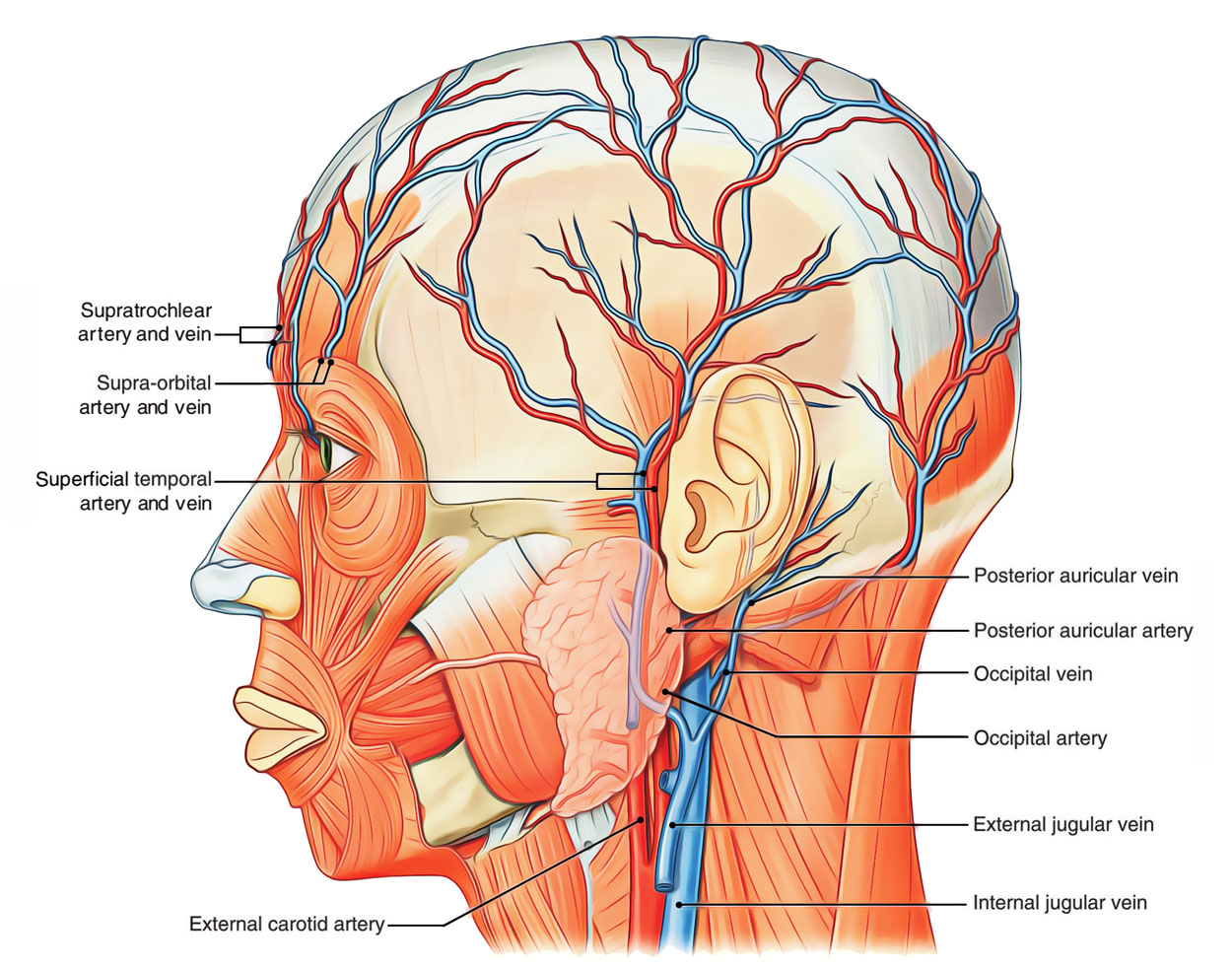
Arterial Supply of Scalp
The scalp has quite abundant blood supply. On every side of midline, it’s supplied by 5 arteries: 3 in front of the auricle and 2 supporting the auricle.
Arteries Supplying the Scalp
| In front of the auricle (from before backwards) | Behind the auricle (from before backwards) |
|---|---|
| Supratrochlear, a branch of ophthalmic artery from internal carotid artery | Posterior auricular artery, a branch of external carotid artery |
| Supraorbital, a branch of ophthalmic artery from internal carotid artery | Occipital artery, a branch of external carotid artery |
| Superficial temporal, a branch of external carotid artery | |
Site of Entrance of Arteries in the Scalp
- Supratrochlear artery enters the scalp around supraorbital margin 1 -finger breadth lateral to the midline.
- Supraorbital artery enters the entire scalp via supraorbital notch 2-3 cm lateral to the supratrochlear artery.
- Superficial temporal artery (the smaller terminal branch of the external carotid), enters the entire scalp in front of the root of zygoma and divides into anterior and posterior branches.
- Posterior auricular artery enters the entire scalp supporting the root of the ear.
- Occipital artery enters the scalp midway between the ear and the external occipital protuberance.
The initial 2 arteries are the branches of ophthalmic artery from internal carotid artery while afterwards 3 arteries are the branches of external carotid artery. The arteries of 1 side freely anastomose with 1 another. There’s also cross anastomosis between the arteries of 2 sides. So the scalp is also the site of potential collateral circulation between the external and internal carotid arteries.
Clinical Significance
The scalp wounds bleed profusely but heal quicklydue to high vascularity. The avulsed portions of scalp, hence, shouldn’t be cut away instead they ought to be set in position and stitched. Since all the arteries supplying the scalp goes into it from below at the periphery, (i.e., from face and neck) the flaps of scalp during craniotomy are made by incisions supplied in the middle and reflected in the direction of the periphery; therefore conserving their blood supply. To ensure the blood supply of the entire scalp, the skin incisions ought to be placed in this style the base of the flap comprises the stalk of 1 of the arteries supplying the entire scalp. Since all the superficial arteries supplying the scalp ascend from face and neck. For that reason life threatening scalp-hemorrhage can be stopped as a first aid measure, by encircling the head just above the ears and eyebrows using a cord or powerful strap of cotton and tied snugly.
Venous Drainage
The scalp on every side of the midline is emptied by 5 veins. The veins of the scalp accompany the arteries and have similar names. All these are as follows:
- Supratrochlear and supraorbital veins: They join each other at the medial angle of the eye to create the angular vein, which continues downwards as the facial vein behind the facial artery.
- Superficial temporal vein: It descends in front of tragus to go into the parotid gland where it joins the maxillary vein to create the retromandibular vein, which ends by dividing into anterior and posterior sections. The anterior section unifies with all the facial vein to create common facial vein, which empties into the internal jugular vein.
- Posterior auricular vein: It descends behind the auricle and connects with the posterior section of the retromandibular vein to create the external jugular vein, which empties into the subclavian vein.
- Occipital vein: It ends in the suboccipital venous plexus.
The veins of the scalp convey with intracranial dural venous sinuses via emissary veins.
Emissary Veins
The veins attaching the veins outside the cranium with the intracranial dural venous sinuses by passing through foramina in the cranium are named emissary veins. Emissary Veins in the Region of the Scalp On every side of the midline in the region of the scalp two sets of emissary veins are seen, viz.
Parietal emissary vein, which goes through parietal foramen and interacts with all the superior sagittal sinus.
Mastoid emissary vein, which goes through mastoid foramen and interacts with all the sigmoid sinus.
Clinical Significance
In babies, the veins of the scalp are easily observed deep to the skin, therefore they’re the preferred sites for intravenous infusion. Diploic veins are thin walled. They’re devoid of valves and drain the diploe of some cranial bones. They start to develop with diploe at about 2 years old. Radiologically they might be viewed as comparatively translucent bands, 3-4 mm wide.
Lymphatic Drainage
The lymphatics from anterior part of the entire scalp with the exception of the lower half of the brow drain into preauricular (or superficial parotid) lymph nodes situated on the face of the parotid gland. The lymphatics from posterior part of the scalp drain into posterior auricular (mastoid) and occipital lymph nodes.

 (82 votes, average: 4.76 out of 5)
(82 votes, average: 4.76 out of 5)