Testis
The Testis is situated in every half of the scrotal sac. It is a male gonad that is homologous with the ovary in the female. Testis is one of the mobile organs of the body. It possesses the various functions, such as – generation of spermatozoa and secretion of testosterone or dihydrotestosterone (a male hormone), it is responsible for the development and maintenance of the secondary sex characteristics of the maleness.
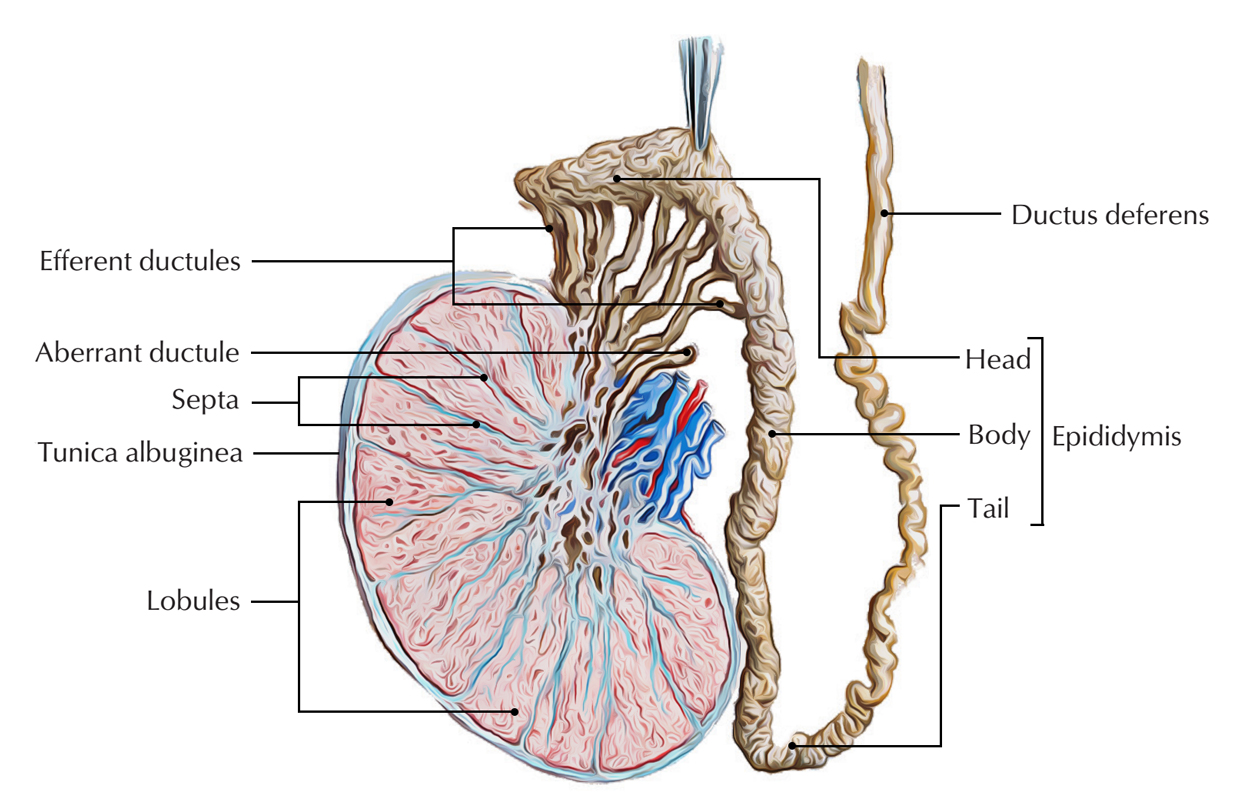
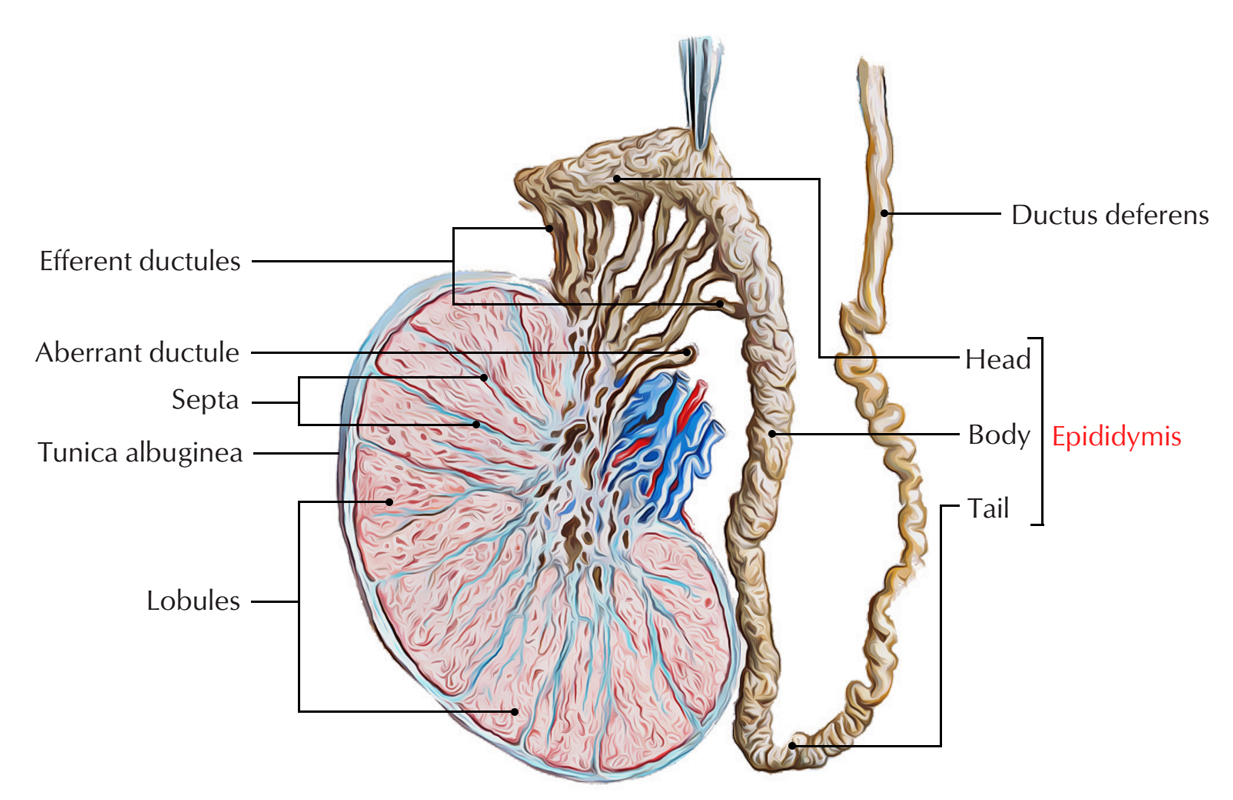
Testis and Epididymis
Shape and Measurements
Shape
It’s oval/ellipsoid in shape (compressed from side to side).
Measurement
It measures roughly 4 X 3 X 2.5 cm (length = 4 cm, width = 2.5 cm, anteroposterior diameter = 3 cm) and weight = 10-15 grams.
Position in the Scrotum
The testis is suspended in the scrotum by the spermatic cord. It is located obliquely, so that its upper pole is leaned somewhat forwards and laterally, and lower post backwards and medially.
The left testis is located somewhat at the lower level compared to the right since the left spermatic cord is somewhat longer in relation to the right. This is because descent of left testis starts early.
External Features
The testis presents the following external features:
- 2 Poles- upper and lower.
- 2 edges- anterior and posterior.
- 2 surfaces- medial and lateral.
Both the upper and lower Poles are convex and smooth. The upper post gives connection to the spermatic cord. The anterior border is rounded and totally covered by the tunica vaginalis. The posterior border is straight and covered only partially by the tunica vaginalis. It gives connection to the epididymis. On the lateral aspect the epididymis is divided from the testis by the expansion of the cavity of tunica vaginalis termed sinus of the epididymis.
Both the medial and lateral surfaces are smooth and somewhat convex.
A small oval body is frequently seen connected to the upper pole of the testis. It’s termed appendix of the testis and symbolizes the remnant of the paramesonephric duct.
Coverings
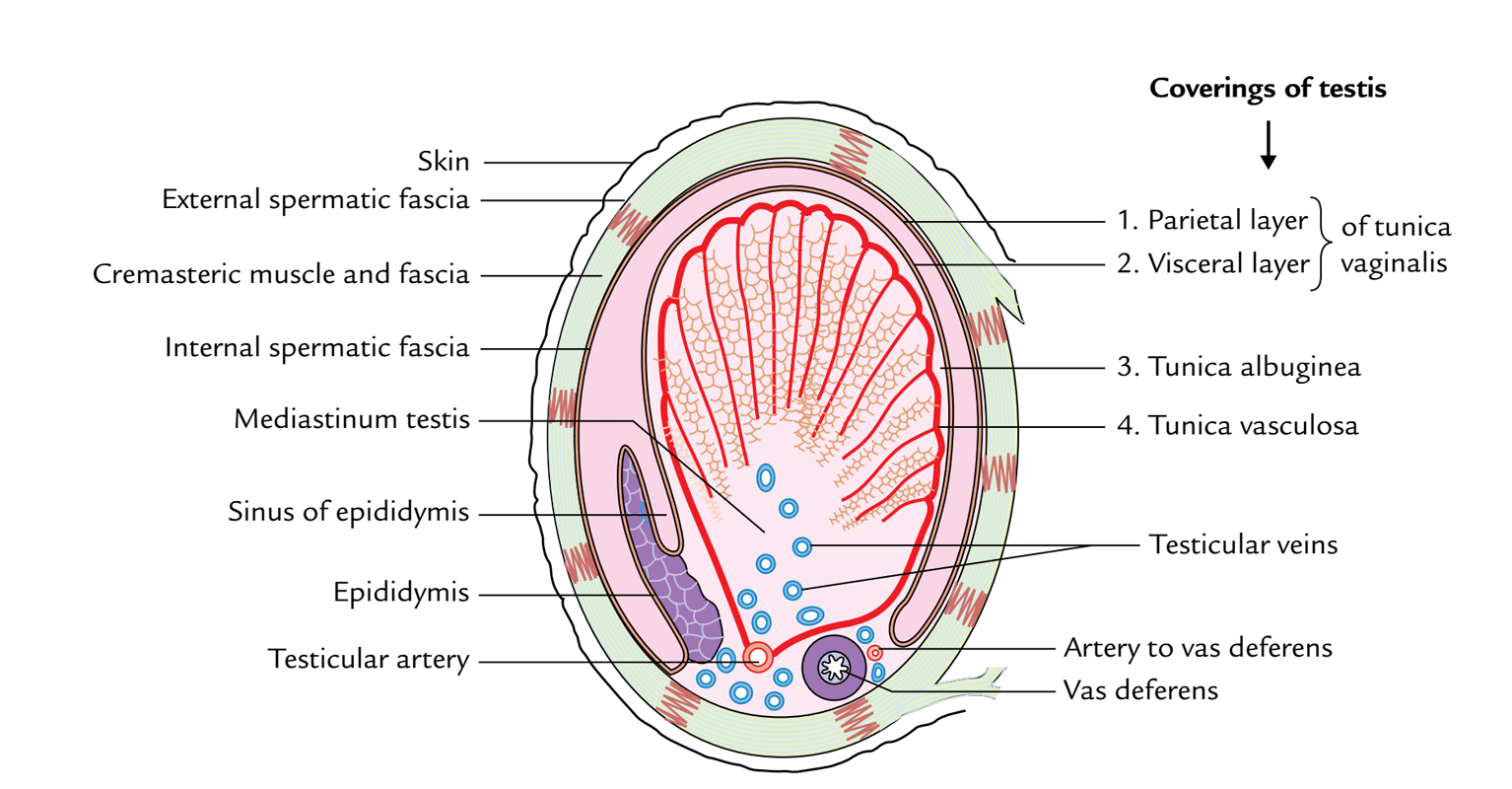
Testis and Epididymis: Coverings
3 jackets cover the testis. From superficial to deep these are:
- Tunica vaginalis.
- Tunica albuginea.
- Tunica vasculosa.
- Tunica Vaginalis.
It’s a serous sac representing the constant lower portion of the processus vaginalis. It’s invaginated by the testis from behind. Consequently, it presents parietal and visceral layers using a potential cavity between them.
Therefore, the tunica vaginalis fully encloses the testes on the front and sides.
Clinical Significance
Hydrocele
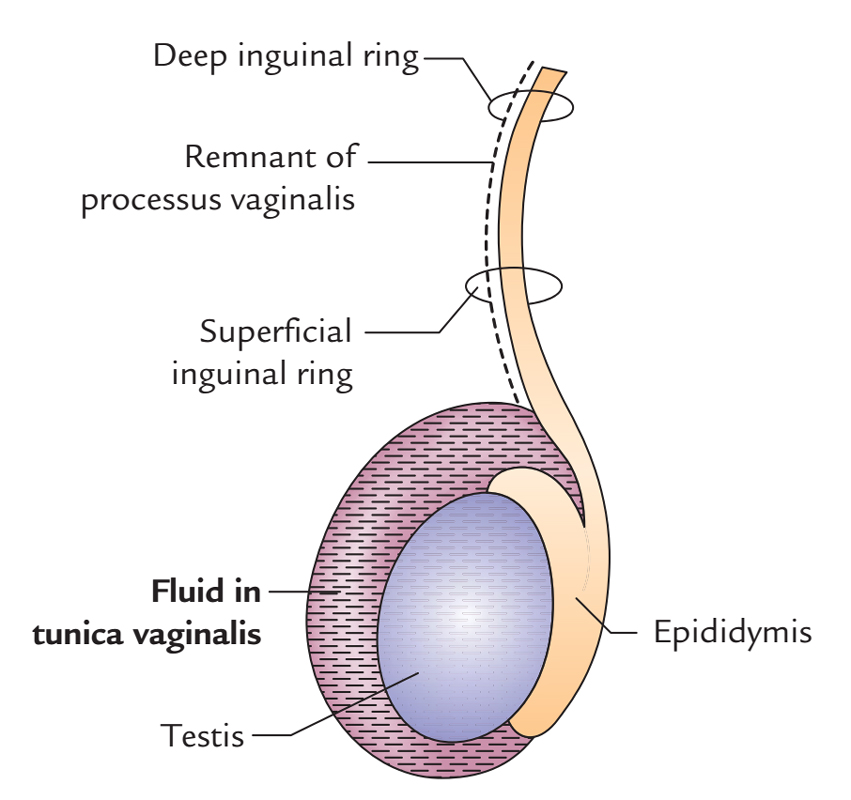
Testis and Epididymis: Hydrocele
It’s the accumulation of the fluid inside the tunica vaginalis. The fluid may accumulate following inflammation of the testis because tunica vaginalis is closely associated with the front and side of the testis but most hydroceles are idiopathic. The fluid from tunica vaginalis can be taken out by adding an excellent trocar and canula via the scrotal skin.
The canula traverses the following structures: (a) skin, (b) dartos muscle, (c) external spermatic fascia, (d) cremasteric muscle and fascia, (e) internal spermatic fascia, and (f) parietal layer of the tunica vaginalis.
The collection of blood and pus in the tunica vaginalis is named hematocele and pyocele, respectively.
Tunica Albuginea
It’s a thick, dense layer of fibrous tissue enclosing the testis. It’s covered by the visceral layer of tunica vaginalis with the exception of where it’s in direct contact together with the epididymis (i.e., superiorly and posteriorly).
Tunica Vasculosa
It’s the innermost vascular layer of the testis, lining the lobules of the testis.
Structure
The testis is enclosed in a fibrous capsule, the tunica albuginea. Posteriorly, the tunica albuginea is thickened to create an incomplete vertical septum/ridge, the mediastinum testis. Numerous incomplete fibrous septa go from the mediastinum to the inner aspect of the tunica albuginea and split the inner part of the testis into 200-300 lobules. Every lobule includes 2 to 4 coiled seminiferous tubules, lined by thick multilayered germinal epithelium that creates spermatozoa. The thin, threadlike loops of seminiferous tubules join every other and become straighter as they pass toward the mediastinum creating straight tubules. The straight seminiferous tubules usually do not generate spermatozoabut eliminate them into the network of stations named the rete testis. The small efferent ductulesconnect the stations of rete testis to the upper end of the epididymis. The interstitial cells, which produce male sex hormones, is located in the areolar tissue between the seminiferous tubules.
Number of lobules in testis: 200-300. Number of seminiferous tubules in every lobule: 2-4. Length of every seminiferous tubule: 60 cm. Therefore, if all the seminiferous tubules are joined together, their overall length becomes 500 m.
Arterial Supply
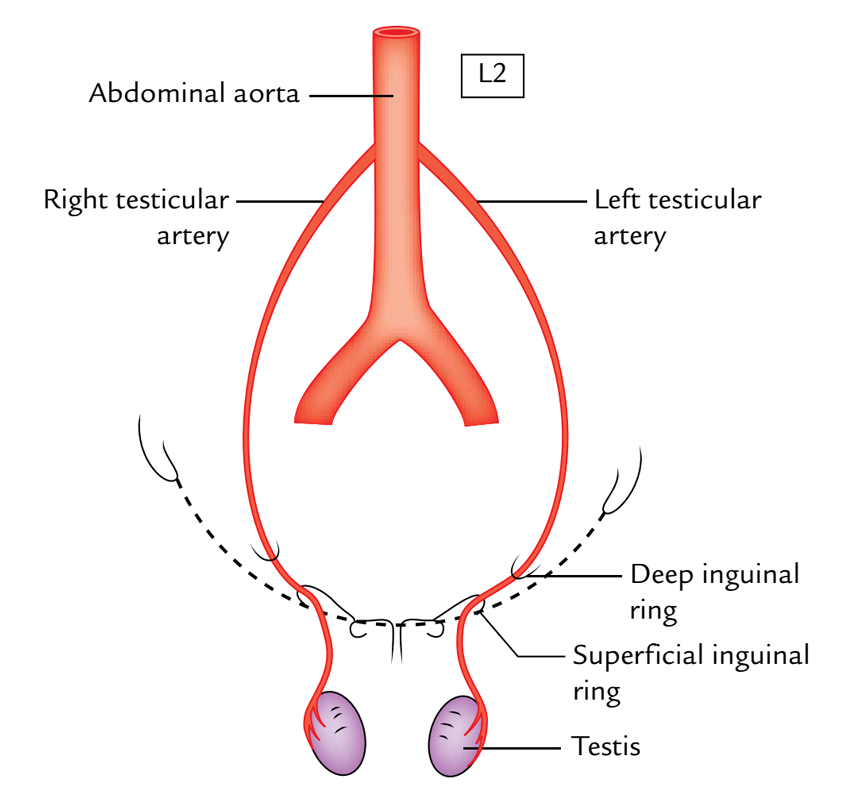
Testis and Epididymis: Arterial Supply
The testicular artery provides the testis, which originates from the abdominal aorta in the abdomen in the level of L2 vertebra. Afterward it enters downward and laterally to goes into the deep inguinal ring, traverses via the inguinal canal inside the spermatic cord to get to the testis. At the posterior border of testis, it’s split into a number of small branches and 2 large (medial and lateral) branches. The medial and lateral branches pierce the tunica albuginea, and ramify on the surface of lobules of the testis to create the tunica vasculosa.
Venous Drainage
The pampiniform plexus of veins (the veins appearing from the testis create a plexus of veins referred to as pampiniform plexus) empties the venous blood from the testis. This plexus ascends up and at the superficial inguinal ring condenses to create 4 veins, which go through the inguinal canal inside the spermatic cord. At the level of deep inguinal ring, they join to create a 2 testicular veins which accompany the testicularartery. On the right side, the testicular vein drains into the inferior vena cava for an oblique angle while on the left side it drains into the left renal vein at a right angle.
Clinical Significance
Varicocele
It’s a clinical state where veins of the pampiniform plexus become dilated, tortuous, and elongated. It generally impacts the teenagers and young adults. It mainly takes place on the left side because of the following reasons: (a) left testicular vein drains at a right angle in the left renal vein for this reason venous pressure is high in the left testicular vein, (b) compaction of the left testicular vein by filled constipated sigmoid colon, and (c) blockage of entrance of the left testicular vein in the left renal vein occasionally may happen by growing malignant tumor of the left kidney.
Medically varicocele gifts as:
- Obscure, pulling sensations and aching pain in the scrotum.
- On palpation, the veins of pampiniform plexus feel like ‘bag of worms’.
It’s must for clinicians to investigate the left kidney in quickly growing left-sided varicocele.
Lymphatic Drainage
The lymph vessels from the testis ascend along the testicular vessels in the spermatic cord and drain into pre-aortic and para-aortic group of lymph nodes at the level of the next lumbar vertebra.
The testicular arteries originate in the abdomen, the testicular veins drain in the abdomen, and testicular lymph vessels drain in the abdominal lymph nodes. This is because during development the testis has migrated from high up on the posterior abdominal wall, down via the inguinal canal into the scrotum, hauling its blood supply and lymph vessels along it.
Epididymis
The epididymis is a comma-shaped structure, which is located on to the superior and posterolateral outermost layer of the testis. It’s created from highly coiled tubes.
Testis and Epididymis: Epididymis
Parts
The epididymis from above downward is split into 3 parts: head, body, and tail.
The head (the upper increased part) is linked to the upper post of testis by efferent ductules and is composed of highly coiled efferent ductules. The body (middle part) and tail (lower span part) are created from a single highly coiled duct of epididymis, which appears from the tail as the vas deferens.
Functions
The functions of epididymis are:
- Storage and maturation of spermatozoa.
- Absorption of the fluid.
- Inclusion of materials to the seminal fluid to nourish the maturating spermatozoa.
Laterally, a distinctive groove exists between the testis and the epididymis. A fold of visceral layer of tunica vaginalis invaginates it to create the sinus of epididymis.
Clinical Significance
Tumors of The Testis
- The 2 primary types of testicular tumors are seminoma (carcinoma of the seminiferous tubules) and teratoma (malignant change in the totipotentcells). The cancer cells from testis propagate upward through the lymph vessels to the lumbar (pre and para-aortic) lymph nodes at the level of L1/L2 vertebra and create secondary tumor in the abdomen.
Torsion of The Testis
It’s a clinical state where rotation of the scrotum happens around the spermatic cord inside the scrotum. It usually impacts the energetic young people and youngsters, and is escorted by acute pain.
- It’s covered by the peritoneum only anteriorly and to the left.
- Posteriorly it’s related to the posterior vagal trunk and the diaphragm.
- Anteriorly it’s related to the anterior vagal trunk and the left lobe of the liver.
- The esophageal branches of the left gastric artery and accompanying veins run along its left side.
The veins from the abdominal part of the esophagus drain partially into the portal vein and partially into the systemic circulation. The veins drain into the portal vein circulation via the left gastric vein and in the systemic circulation via the hemiazygos vein. So, it’s 1 of the significant ssites of portocaval anastomosis.
Esophageal Varices
The lower end of the esophagus is 1 of the significant ssites of portocaval anastomosis. In portal hypertension (example, because of cirrhosis of the liver), the portocaval anastomotic channels open and become dilated and tortuous creating esophageal varices. Their rupture can cause serious and deadly hematemesis (vomiting of blood).
Achalasia Cardia
As a result of neuromuscular incoordination occasionally the lower end of the esophagus fails to open and doesn’t enable easy passage of food resulting in dysphagia named achalasia cardia. Marked dilatation of the esophagus may take place because of accumulation of food inside it.
The lower end of the esophagus is inclined for inflammation and ulceration because of acidic regurgitation from the stomach.
The lower end of the esophagus is the commonest site of carcinoma.
Development of Testis and Epididymis
The testis develops in the abdominal cavity on its posterior wall from the genital ridge on the medial side of the developing (mesonephros at the level of T10 segment. All the components of the testis (tunica albuginea, fibrous septa, seminiferous tubules, straight tubules, rete testis, and Sertoli cells) develop from the genital ridge except primordial germ cells (spermatogonia), which develop from the wall of yolk sac and migrate secondarily into the genital ridge.
Most of the mesonephric tubules atrophy, but about 10-15 tubules persist and form the efferent ductules of the testis.
The mesonephric duct forms the duct of epididymis, vas deferens, seminal vesicles, and ejaculatory duct.
Embryological Remnants in Relation to Testis and Epididymis
These are as follows:
- Appendix of testis: It is an oval body attached to the upper pole of testis.
- Appendix of epididymis (hydatid of Morgagni): It is a small pedunculated rounded body attached to the head of epididymis. It is remnant of cranial end of mesonephric (Wolffian) duct.
- Paradidymis (organ of Giraldes): It consists of 3 or 4 small free tubules which are found in the spermatic cord, just above the head of epididymis. They are remnants of caudal mesonephric tubules.
- Superior aberrant ductules: They are 2 or 3 in number and attached to the upper end of testis above the afferent ductules of testis. They are remnants of the upper mesonephric tubules.
- Inferior aberrant ductules: They are 1 or 2 in number and attached to the tail of epididymis. They are remnants of the intermediate mesonephric tubules.
The embryological remnants (vide supra) may sometime form cysts in relation to the testis and epididymis.
Descent of the Testis
The testis develops in the abdominal cavity where the temperature is high and not suitable for proper spermatogenesis. Hence, it migrates out of the abdominal cavity into the scrotum.
At an early stage of intrauterine life, the developing testis lies in the upper abdomen on the medial side of the mesonephros. A fold of the peritoneum called processus vaginalis extends in front of the testis and reaches the scrotum. Just after the formation of processus vaginalis, a cord-like fibromuscular band, the gubernaculum testis, develops and connects the mesonephric duct, and the lower pole of the testis to the base of the scrotum. Differential body growth in the embryo and fetus results in the descent of the testis from the abdominal cavity to the scrotum.
Each testis begins to descend during the 2nd month of the intrauterine life (IUL).
- It reaches the iliac fossa by the 3rd month of IUL.
- It rests at the deep inguinal ring from 4th to 6th month of IUL.
- It traverses the inguinal canal during the 7th month and reaches the superficial inguinal ring by the 8th month of IUL.
- It enters the scrotum at the 9th month of IUL
- It reaches the base of the scrotum at or just after birth.
Factors Responsible for Descent of the Testis
These factors are as follows:
- Differential growth of the body wall.
- Increased intra-abdominal pressure and temperature.
- Hormones (male sex hormones produced by the testis, and maternal gonadotrophins).
- Contraction of the gubernaculum (a band of loose fibromuscular tissue extending from the lower pole of the testis to the base of the scrotum).
- Calcitonin gene-related peptide (CGRP), a neurotransmitter secreted by the genitofemoral nerve.
Clinical Significance
The testis may be subject to the following congenital anomalies:
Cryptorchidism (Incomplete Descent of Testis)
In this condition, the testis, during its descent, although it travels through its normal path but fails to reach the base of the scrotum. Thus, it may be found (a) within the abdomen, (b) at the deep inguinal ring, (c) within the inguinal canal, (d) at the superficial inguinal ring, or (e) high up in the scrotum.
The complications of cryptorchidism are:
- It may fail to produce spermatozoa.
- It is prone to undergo malignant change.
Ectopic Testis (Maldescent of the Testis)
- In this condition, the testis travels down along an abnormal path, and therefore fails to reach the scrotum. Thus, it may be found (a) in the superficial fascia of the lower part of the anterior abdominal wall, (b) in front of the pubis, (c) in the perineum, or (d) in the thigh.
- In the past the ectopic testis was attributed to the gonad following a subsidiary tail of gubernaculum. But now it is felt that it occurs because processus vaginalis reaches an abnormal site and testis follows it.
- It is necessary for the testis to be in the scrotum for proper spermatogenesis. Therefore, it is necessary that the undescended testis is brought down in the scrotum (by a surgical procedure) before puberty.
- An ectopic testis usually develops normally, but it is susceptible to trauma. Therefore, it should also be placed in the scrotum by a surgical procedure.

 (53 votes, average: 4.51 out of 5)
(53 votes, average: 4.51 out of 5)