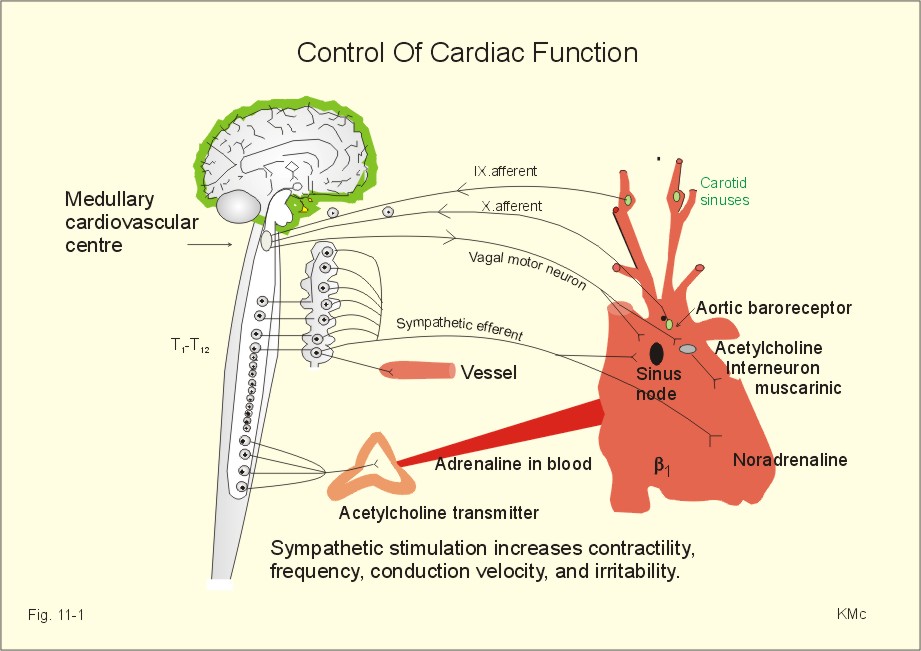
Heart rate regulation is primarily under the control of the cardiac control center located within the medulla oblongata of the brain. It receives sensory information about the level of blood pressure from baroreceptors located in the aortic arch and the carotid sinuses of the internal carotid arteries. It also receives sensory information from chemo- receptors in the aortic arch and the carotid bodies of the external carotid arteries. Baroreceptors are sensitive to changes in vessel wall stretching caused by both high and low blood pressure. Chemoreceptors are stimulated by low blood pH, high blood carbon dioxide levels, and very low blood oxygen levels. The cardiac control center is also affected by emotions, which are generated by the limbic system. The cardiac control center consists of both sympathetic and parasympathetic components. Nerve impulses transmitted to the heart via sympathetic axons cause an increase in heart rate and contraction strength, while nerve impulses transmitted by parasympathetic axons cause a decrease in heart rate. The cardiac control center constantly adjusts the frequency of sympathetic and parasympathetic nerve impulses to produce a heart rate and a contraction strength that meets the changing needs of tissue cells.
Cardiac sympathetic nerves (SNS) originate from spinal nerves C-7 to T-6, pass to the stellate ganglion, then to the epicardial plexus. The right epicardial plexus, with norepinephrine as the neurotransmitter, innervates the SA node. Norepinephrine increases heart rate. Elevated temperature and stretch also can act directly on the SA node to increase heart rate. The left epicardial plexus innervates the AV node, at which norepinephrine increases conduction velocity.
The external environment of the heart also influences myocardial performance. Endocrine agents with cardiac actions include the adrenal catecholamines epinephrine and norepinephrine, whose actions mimic those of the cardiac sympathetic nerve; thyroid hormone and growth hormone, which play a nutritive role and set the basal tone of the cardiovascular system; and insulin and glucagon, which both have a direct positive inotropic effect.
Blood gases can directly and indirectly alter cardiac function. Severe hypoxia directly depresses myocardial function. Very high CO2 directly depresses myocardial function, and acidosis decreases Ca++ release from SR and consequently decreases contractility. Indirectly, moderate hypoxia causes activation of the sympathetic nervous system, and increases heart rate, contractility, and therefore cardiac output. Moderate hypercapnia also causes a sympathetic activation and increases heart rate, contractility, and therefore cardiac output.
Cardiac Output
The cardiac output is the volume of blood pumped by the heart each minute. It can be calculated as stroke volume times heart rate. Factors that alter stroke volume or heart rate will change cardiac output. Normally it is about 5 L/min (70 mL/beat x 72 beats/min). Cardiac index is defined as cardiac output/body surface area, and it allows comparisons of cardiac function between individuals of different sizes.
Cardiac output measurements are direct or indirect. Direct determination uses a type of flowmeter. A Doppler flowmeter actually measures velocity, which is converted to an estimation of flow based on the vessel cross-sectional area. Indirect measurement often involves the Fick principle.
Cardiac Output = O2 consumed per minute / Pulmonary venous O2 − pulmonary arterial O2
An indicator dilution technique involves injection of a known amount of dye and measurement of the consequent concentration change downstream. However, dye can accumulate if multiple measurements are taken. Thermal dilution involves injection of cold saline and measurement of the resultant change in temperature downstream. This approach can be performed with a Swan-Ganz catheter and is suitable for multiple determinations.
Improved ventricular imaging techniques allow accurate measurement of ventricular end-diastolic and ventricular end-systolic volumes. Consequently, imaging combined with electrocardiographic measurement of heart rate allows noninvasive measurement of cardiac output and ejection fraction.
CO = SV x HR
At normal resting values of a stroke volume of 70 ml/beat and a heart rate of 72 beats/min, the cardiac output is 5,040 ml/min. This means that the total volume of blood, 4 to 6 liters, passes through each ventricle of the heart each minute. Cardiac output increases with exercise because both stroke volume and heart rate increase.
Heart function is regulated by factors both internal and external to the heart. For example, venous return, the amount of blood returning to the heart during diastole, is an internal factor that affects stroke volume. If venous return increases, more blood enters and is pumped from the ventricles, increasing the stroke volume and cardiac output. Heart rate is primarily controlled externally by the autonomic nervous system, although hormones and certain ions also affect it.
Neurons of the sympathetic division extend axons from the cardiac control center down the spinal cord to the thoracic region. There the sympathetic axons exit the spinal cord to innervate the SA node, AV node, and portions of the myocardium. The transmission of nerve impulses causes the sympathetic axons to secrete norepinephrine at synapses in the heart. Norepinephrine increases the heart rate and strengthens the force of myocardial contraction. Physical and emotional stresses, such as exercise, excitement, anxiety, and fear, stimulate the sympathetic division to increase heart rate and contraction strength.
Parasympathetic axons arise from the cardiac control center and exit in the vagus nerve (CN X) to innervate the SA and AV nodes. The transmission of nerve impulses causes the parasympathetic axons to secrete acetylcholine at the heart synapses, which decreases the heart rate. The greater the frequency of parasympathetic nerve impulses sent to the heart, the slower the heart rate. Excessive blood pressure and emotional factors, such as grief and depression, stimulate the parasympathetic division to decrease the heart rate.
When the heart is at rest, more parasympathetic nerve impulses than sympathetic nerve impulses are sent to the heart. As cellular needs for blood increase, a decrease in the frequency of parasympathetic nerve impulses and an increase in sympathetic nerve impulses cause heart rate to increase.
Other Factors Affecting Heart Function
Age, sex, physical condition, temperature, epinephrine, thyroxine, and the blood levels of calcium and potassium ions also affect the heart rate and contraction strength.
The resting heart rate gradually declines with age, and it is slightly faster in females than in males. Average resting heart rates in females are 72 to 80 beats per minute, as opposed to 64 to 72 beats per minute in males. People who are in good physical condition have a slower resting heart rate than those in poor condition. Athletes may have a resting heart rate of only 40 to 60 beats per minute. An increase in body temperature, which occurs during exercise or when feverish, increases the heart rate.
Epinephrine, which is secreted by the adrenal glands during stress or excitement, affects the heart like norepinephrine-it increases the rate and strength of heart contractions. An excess of thyroxine produces a lesser, but longer-lasting, increase in heart rate.
Reduced levels of blood Ca2+ decrease the rate and strength of heart contraction, while increased levels of blood Ca2+ increase heart rate and contraction strength, and prolong contraction. In extreme cases, an excessively prolonged contraction may result in death. Excessive levels of blood K+ decrease both heart rate and contraction strength. A high dose of K+ is often used in lethal injections, in which the abnormally high levels of blood K+ cause the heart to stop contracting. Abnormally low levels of blood K+ may cause potentially life-threatening abnormal heart rhythms.



 (95 votes, average: 3.39 out of 5)
(95 votes, average: 3.39 out of 5)